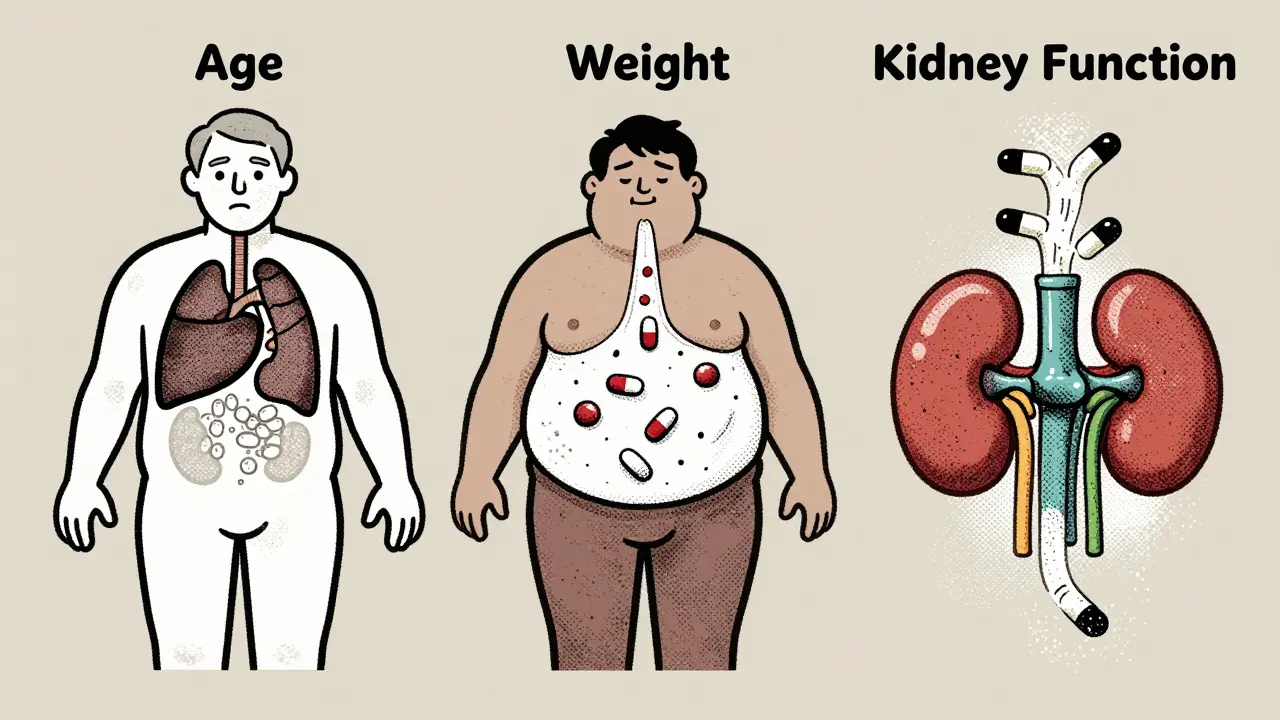
Getting the right dose of medication isn’t just about following the label. For many people, the standard dose on the bottle could be too much-or too little. That’s because how your body handles medicine depends on three key things: your age, your weight, and how well your kidneys are working. Skip these adjustments, and you risk side effects, hospital visits, or even life-threatening reactions. Get it right, and the medicine works as it should-without harm.
Why One Size Doesn’t Fit All
Think of your body like a car. A 20-year-old sports car and a 20-year-old sedan both run on gasoline, but they handle fuel differently. Your body works the same way with drugs. As you age, gain weight, or lose kidney function, your body’s ability to process and clear medications changes. A dose that’s perfect for a healthy 40-year-old might overload an 80-year-old with kidney disease or underdose someone who weighs 130 kg.
According to the National Kidney Foundation, about 1 in 7 adults in the U.S. has chronic kidney disease. That means millions of people are taking medications that their kidneys can’t clear properly. And it’s not just kidney patients. Nearly half of all adults over 65 have reduced kidney function-even if they don’t know it. The same goes for people with obesity or very low body weight. These aren’t rare edge cases. They’re everyday realities.
Age: Slower Clearance, Higher Risk
As you get older, your kidneys naturally lose some of their filtering power. By age 70, most people have lost 30-50% of their kidney function compared to when they were 30. Your liver also slows down. Muscles shrink. Fat increases. All of this changes how drugs move through your body.
Take digoxin, a heart medication. In younger people, it’s cleared quickly. In older adults, it builds up. Too much leads to nausea, confusion, or dangerous heart rhythms. That’s why doctors often cut the dose in half for patients over 70-even if their blood tests look normal.
Another example: benzodiazepines like lorazepam. These are used for anxiety or sleep, but they linger longer in older bodies. The result? Dizziness, falls, broken hips. The American Geriatrics Society recommends avoiding these drugs in seniors unless absolutely necessary. And if they’re used, the dose should be 50% lower than what’s listed on the bottle.
Studies show that 30% of adverse drug events in older adults come from dosing mistakes tied to age-related changes. That’s not just a risk-it’s a pattern.
Weight: Bigger Body, Different Math
Weight matters more than you think. But not in the way you’d expect.
If you’re underweight, your body has less fluid and muscle to spread the drug out. That means a standard dose can become too concentrated. For example, in someone who weighs 45 kg, a normal dose of vancomycin (an antibiotic) can cause hearing damage because the drug builds up too fast.
On the other end, obesity changes how drugs are absorbed and stored. Fat doesn’t soak up water-soluble drugs the way muscle does. So if you’re obese, your body might not get enough of the medicine. But some drugs stick in fat tissue and get released slowly, leading to delayed toxicity.
That’s why doctors use adjusted body weight for dosing, not your actual weight. Here’s how it works:
- Calculate your ideal body weight (IBW): For men, 50 kg + 2.3 kg for every inch over 5 feet. For women, 45.5 kg + 2.3 kg per inch over 5 feet.
- If your BMI is over 30, use this formula: Adjusted weight = IBW + 0.4 × (actual weight − IBW)
For example, a woman who is 5’6” and weighs 100 kg has an IBW of about 63 kg. Her adjusted weight for dosing? 63 + 0.4 × (100 − 63) = 78 kg. That’s the number used to calculate her kidney function and drug dose-not her real weight.
Using actual weight for dosing in obesity can lead to underdosing antibiotics, anticoagulants, or chemotherapy. Underdosing means the treatment fails. Overdosing means toxicity. The difference between success and disaster often comes down to this calculation.

Kidney Function: The Hidden Driver
Your kidneys filter about 120-150 quarts of blood each day. If they’re working at 70%, most drugs are cleared fine. But if they’re at 30%? That’s when problems start.
Over 40% of commonly prescribed drugs are cleared mostly or entirely by the kidneys. That includes:
- Metformin (for diabetes)
- Atorvastatin (for cholesterol)
- Vancomycin and cefazolin (antibiotics)
- Enalapril and lisinopril (blood pressure meds)
- Many painkillers like tramadol and morphine
When kidney function drops, these drugs stick around. That’s why a diabetic patient with an eGFR of 28 can’t safely take 1000 mg of metformin twice daily. The FDA says the max dose at that level is 500 mg once a day. Yet, a 2023 Reddit post from a pharmacist described a patient on that exact wrong dose for six months-until they caught it.
Doctors don’t just look at serum creatinine. They use equations to estimate how well the kidneys are filtering. Two main ones are used:
- Cockcroft-Gault: Calculates creatinine clearance (CrCl) in mL/min. Still used in 85% of drug labels and preferred for dosing, especially in obese patients.
- CKD-EPI: Estimates glomerular filtration rate (eGFR) in mL/min/1.73m². Used for staging kidney disease, not dosing.
Here’s the catch: CKD-EPI is more accurate for most people-but it overestimates kidney function in obese patients by 15-20%. That means if you rely only on eGFR, you might think someone’s kidneys are fine when they’re not. That’s why experts say: Use CrCl for dosing. Use eGFR for staging.
Stages of kidney disease (based on eGFR):
- Stage 1: eGFR ≥90 (normal, but with kidney damage)
- Stage 2: eGFR 60-89 (mild reduction)
- Stage 3a: eGFR 45-59 (mild to moderate)
- Stage 3b: eGFR 30-44 (moderate to severe)
- Stage 4: eGFR 15-29 (severe)
- Stage 5: eGFR <15 (kidney failure)
For dosing: If eGFR is above 60, most drugs don’t need adjustment. Below 60? Check the label. Below 30? Almost all renally cleared drugs need major changes.
Real-World Mistakes and How to Avoid Them
Here are three common errors you won’t find on drug labels:
- Using eGFR to dose drugs: A patient with eGFR 35 might be told their kidneys are “only mildly impaired.” But if the drug is cleared 80% by kidneys, that’s Stage 3b. Dose reduction is needed. Relying on eGFR alone misses this.
- Ignoring body weight in obesity: A pharmacist in Ohio recently caught a 140 kg patient being given a standard dose of enoxaparin (a blood thinner). The dose was too low-by 40%. The patient had a clot the next day.
- Not checking for drug interactions: A patient on metformin and cimetidine (an acid reducer) can have dangerous buildup. Cimetidine blocks kidney clearance of metformin. Even with normal eGFR, this combo can cause lactic acidosis.
Studies show that 68% of pharmacists see inappropriate renal dosing at least once a week. The biggest culprits? Antibiotics, diabetes drugs, and blood pressure meds.
The fix? Use tools. Most hospitals now have electronic alerts that pop up when a dose is wrong. One study found these alerts cut serious errors by 47%. If you’re on a chronic medication, ask your pharmacist: “Is this dose based on my kidney function and weight?”

What You Can Do
You don’t need to be a doctor to protect yourself. Here’s what works:
- Know your eGFR or CrCl. Ask for it at every checkup. It’s not just a lab number-it’s a safety number.
- Keep a list of all your meds, including supplements. Bring it to every appointment.
- If you’re over 65, obese, or have diabetes or high blood pressure, assume your kidney function is lower than it looks. Ask if your doses need adjusting.
- Don’t assume “normal” creatinine means normal kidney function. A creatinine of 1.2 might be fine for a 30-year-old man-but dangerous for a 75-year-old woman.
- If a new drug is prescribed, ask: “Is this dose adjusted for my kidneys and weight?”
Medication safety isn’t about following instructions. It’s about understanding how your body works-and making sure the medicine fits you, not the other way around.
Future of Dosing: What’s Coming
Right now, dosing is based on population averages. But that’s changing.
The FDA is pushing for real-time monitoring. Imagine a wearable device that tracks your kidney filtration rate every hour-like a fitness tracker for your kidneys. Pilot programs are already testing this.
AI tools are being trained to combine your genetics, weight, age, and lab values to give a personalized dose. A $50 million NIH project is testing this in 15 U.S. hospitals starting in late 2024.
By 2025, a new standardized dosing database will launch-finally ending the confusion between hospital formularies that give five different doses for the same drug.
But until then, the rules stay the same: Check your kidney function. Adjust for weight. Respect age. Your life might depend on it.
9 Comments
John McDonaldFebruary 9, 2026 AT 03:38
Been on metformin for 12 years and just found out my kidney numbers dropped last year. Doc didn’t mention adjusting my dose until I brought it up. Seriously, how many people are just winging it with meds? This post is a wake-up call.
My grandma got hospitalized because her blood pressure med wasn’t adjusted after her stroke. She was fine for years, then boom-low blood pressure, passing out, ambulance. All because they used the same dose.
Doctors need to stop treating us like robots with preset settings. We’re not all 30-year-old gym bros.
Also, love the car analogy. My 2005 Corolla and my buddy’s 2023 Tesla both use gas, but you don’t put 20 gallons in the Corolla and expect it to run better. Same logic.
Chelsea CookFebruary 9, 2026 AT 16:50
Oh wow, so the medical industry finally figured out that not everyone is a 170 lb 25-year-old male? Took them long enough.
My sister’s a nurse. She told me once that 70% of med errors in elderly patients are from ‘standard dosing.’ Like, who wrote the label? A 22-year-old med student on caffeine and regret?
Andy CortezFebruary 9, 2026 AT 21:30
lol so you’re telling me my 6’4” 280 lb ass can’t just take the same oxycodone as my cousin who’s 5’5” 110 lbs? I mean… I knew that already but like… why is this even a thing? Are we still using dosing charts from 1987?
Also, cockcroft-gault? sounds like a failed band name. I’d listen to that album though.
and why does everyone keep saying ‘kidney function’ like it’s a wifi signal? ‘My kidneys are at 45%… I think I need to reboot them.’
Jacob den HollanderFebruary 10, 2026 AT 16:06
This is so important. I’ve seen too many elderly patients get confused because their meds weren’t adjusted. One man was on lisinopril for years, then his kidney function dipped to Stage 3b. He didn’t know. His doctor didn’t adjust. He ended up with hyperkalemia, ended up in the ER.
It’s not just about the numbers-it’s about communication. Families need to know. Patients need to know. Pharmacists need to be louder.
And yes, adjusted body weight is a game-changer. I had a patient who was obese, took the full dose of vancomycin, and ended up with ringing in her ears for months. It was preventable.
Thank you for writing this. We need more of this kind of clarity.
Also, the Cockcroft-Gault vs eGFR point? YES. So many docs mix them up. I’ve had to correct pharmacy orders before. It’s wild.
Andrew JacksonFebruary 11, 2026 AT 16:13
It is a disgrace that modern medicine has devolved into this kind of relativistic, identity-based dosing. There was a time when a pill was a pill, and a man took what was prescribed, regardless of his ‘weight’ or ‘age.’
Now we are told to adjust for everything-gender, BMI, ethnicity, kidney function. This is not science. This is social engineering masquerading as pharmacology.
When I was a young man in 1983, we didn’t ask for permission to take medicine. We took it. And we didn’t get sick. Why? Because we had discipline. Not spreadsheets.
Stop coddling people. A dose is a dose. The body adapts. Or it doesn’t. That’s nature. Not a spreadsheet.
Joseph Charles ColinFebruary 12, 2026 AT 09:28
Let’s clarify a few key pharmacokinetic principles here. Renal clearance is primarily governed by glomerular filtration rate (GFR) and tubular secretion, not total body weight per se. The Cockcroft-Gault equation accounts for serum creatinine, age, and sex-making it more accurate for drug dosing than eGFR in clinical practice, especially in non-steady-state scenarios.
For obese patients, the adjusted body weight (ABW) model-specifically, IBW + 0.4*(actual − IBW)-is validated for aminoglycosides, vancomycin, and beta-lactams. However, for lipophilic agents (e.g., lorazepam, diazepam), volume of distribution is more influenced by fat mass, necessitating lean body weight or total body weight depending on the drug’s logP.
Metformin’s FDA labeling is based on eGFR thresholds, but real-world data from the UK Clinical Practice Research Datalink shows that even at eGFR 30–45, dosing at 1000 mg BID carries <5% risk of lactic acidosis if no contraindications exist.
Bottom line: context matters. Algorithms help, but clinical judgment > formula.
Joshua SmithFebruary 12, 2026 AT 23:52
I’m a pharmacy tech and this is spot on. We had a guy come in last week on 1000mg metformin twice a day. His eGFR was 29. We called his doctor. They didn’t even know. Said they just ‘followed the script.’
It’s scary how often this happens. We’re not just filling prescriptions-we’re safety nets. But we shouldn’t have to be.
Also, the weight thing? My aunt is 5’2” and 190 lbs. She was on the same blood thinner as her 130 lb sister. One had a bleed. The other was fine. It’s not fair to the patient or the provider.
Randy HarkinsFebruary 13, 2026 AT 13:43
Thanks for this. My dad’s on 4 meds and I just realized none of them were adjusted after his kidney scan last year. I’m taking this to his next appointment. He’s 78, weighs 210, and has been on the same dose since 2018. 😬
Also, love the car analogy. My Prius and my brother’s F-150 both need gas, but you don’t put 20 gallons in the Prius. Same logic. 👍
Elan RicarteFebruary 15, 2026 AT 12:10
Ohhhhh so THAT’S why my cousin’s grandma died from a heart attack after taking digoxin? She was on the same dose as her 40-year-old son. Like, what the actual fuck? This isn’t medicine-it’s Russian roulette with pills.
And don’t even get me started on how doctors treat obesity like a moral failing. ‘Oh, you’re obese? Here’s a 50% dose reduction.’ No, you dumbass-her fat tissue is a drug sponge, not a sin. Adjust the math, not the shame.
Also, cockcroft-gault? Sounds like a medieval torture device. I’m surprised it’s still in use. Should be called ‘the old man’s calculator.’
And why are we still using ‘ideal body weight’? That’s a 1970s concept. Who decided that 5’6” women should be 63kg? That’s not ideal, that’s a Pinterest aesthetic.
Also, why is no one talking about how this system punishes people who don’t fit the ‘average’ mold? Like, what if you’re 5’1” and 80kg? Or 6’7” and 140kg? Are you just supposed to die quietly? This is broken.