When you take cannabis along with a sleeping pill, painkiller, or anti-anxiety medication, you’re not just adding two effects-you’re multiplying them. The combination doesn’t just make you drowsy. It can slow your breathing to dangerous levels, leave you confused or unconscious, and in rare cases, kill you. This isn’t speculation. It’s documented in emergency rooms, clinical studies, and patient reports across the U.S. and Europe.
How Cannabis Acts Like a CNS Depressant
Cannabis isn’t just a recreational drug or a natural remedy-it’s a central nervous system (CNS) depressant. That means it slows down brain activity, just like alcohol, benzodiazepines, barbiturates, and opioids. The main active ingredient, delta-9-tetrahydrocannabinol (THC), binds to CB1 receptors in the brain, reducing nerve signaling. This leads to relaxation, reduced anxiety, and sleepiness-but also dizziness, slurred speech, memory gaps, and trouble focusing.
These effects start fast if you smoke or vape: within minutes, peak at 30 minutes, and fade in 2-4 hours. If you eat it-like gummies or brownies-it takes 30 to 90 minutes to kick in, lasts 6-8 hours, and hits harder. Even small doses of THC (5-10 mg) can impair reaction time and attention. And unlike what some think, this isn’t just a beginner thing. Experienced users see the same cognitive slowdown, just with less panic.
The Real Danger: Additive Sedation
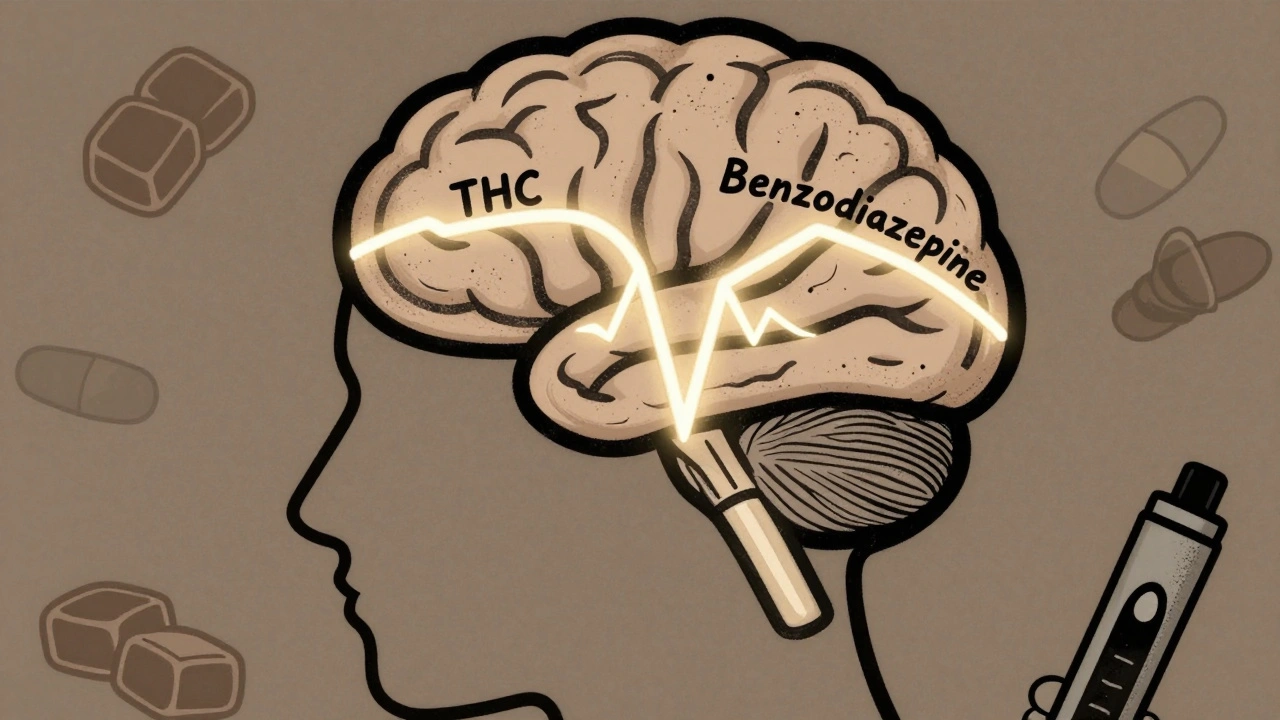
Here’s where it gets risky. When you mix cannabis with other CNS depressants, the effects don’t just add up-they multiply. This is called additive sedation. A 2020 study in The British Journal of Psychiatry found that cannabis impairs cognitive function in ways nearly identical to alcohol and benzodiazepines. When combined, the result is worse than either alone.
Take benzodiazepines like Xanax or Valium. Both work by boosting GABA, a brain chemical that calms neural activity. Cannabis does something similar through its own system. When you stack them, your brain gets hit with double the calming signals. The outcome? Extreme drowsiness, confusion, and dangerously slow breathing.
One Reddit user, u/AnxietyWarrior, described waking up on the bathroom floor after taking half a milligram of Xanax and one hit of 20% THC flower. His oxygen levels dropped to 82%. He had no memory of how he got there. That’s not an outlier. In 2022, U.S. emergency rooms recorded over 7,800 visits involving cannabis and benzodiazepines-a 42% jump from 2019.
Why Opioids Are Especially Dangerous
Combining cannabis with opioids like oxycodone or fentanyl is even more perilous. Both suppress breathing, but through different pathways. Cannabis reduces the brain’s drive to breathe. Opioids directly paralyze the respiratory centers. Together, they create a multiplicative risk-not just additive.
A 2020 study in the Journal of Clinical Medicine found that people using both cannabis and opioids had a 3.2 times higher chance of ending up in the ER. Over two-thirds of those visits involved breathing problems. The CDC updated its opioid prescribing guidelines in 2022 to explicitly warn that cannabis can make opioids more dangerous. Doctors now have to ask patients: Are you using marijuana? Not just for pain, but for sleep, anxiety, or stress?

What the Experts Are Saying
Medical organizations aren’t mincing words. The American Society of Anesthesiologists says anyone using cannabis within 72 hours of surgery needs close monitoring. Anesthesia is a CNS depressant. So is cannabis. Combine them, and you risk needing more drugs to get you asleep-and then struggling to wake up safely.
Dr. Evan S. Kharasch from Washington University found that cannabis users needed 20-25% more propofol (a common IV anesthetic) to get the same effect. But they also had 37% more breathing problems after surgery. That’s not a coincidence. It’s biology.
The American Academy of Neurology and the American Medical Association both say doctors must screen for cannabis use before prescribing any depressant. The American Society of Health-System Pharmacists even created a risk-scoring tool. It gives points for THC strength (up to 5), type of depressant (opioids = 4 points, barbiturates = 5), and patient age (65+ = 2 points). A score above 7 means high risk-and you should reconsider the combination.
Who’s Most at Risk?
Older adults are especially vulnerable. Many take opioids for arthritis, benzodiazepines for insomnia, and now turn to cannabis for pain or anxiety. They’re often on multiple meds already. Their bodies process drugs slower. Their lungs and brains are less resilient. A 2022 survey of 1,247 medical cannabis users found that nearly 4 out of 10 were also using prescription CNS depressants. Over 22% had experienced an episode of extreme sedation-enough to require medical help.
But it’s not just seniors. Young adults using cannabis for anxiety and then grabbing a sleeping pill after a bad night are equally at risk. The myth that “natural” means “safe” is deadly here. Cannabis isn’t harmless. Especially when it’s high-THC. Products over 10% THC increase the chance of paranoia and confusion. Over 15%? That’s where the real danger spikes.
What About CBD?
Not all cannabis is the same. CBD-dominant products-with little to no THC-appear to carry far less risk. A 2022 trial in JAMA Internal Medicine tested 127 people taking high-CBD oil (150 mg CBD, less than 0.3% THC) with alprazolam (Xanax). No significant interaction was found. That’s promising. But it’s not a green light. Most CBD products on the market aren’t pure. They contain trace THC. And we still don’t know how CBD interacts with all depressants long-term.
For now, if you’re using CBD for anxiety or pain and also take a depressant, talk to your doctor. Don’t assume it’s safe just because it’s labeled “CBD.”
What Should You Do?
If you’re using cannabis and a CNS depressant, here’s what to do:
- Don’t mix them without medical supervision. Even if you feel fine, your breathing may be slowing without you noticing.
- Avoid high-THC products. Stick to products under 10% THC if you must use both. Lower is safer.
- Space out doses. The National Institute on Drug Abuse recommends waiting at least 4 hours between taking cannabis and another depressant. But even that doesn’t eliminate risk.
- Start low and go slow. If you’re new to either, use the smallest possible dose first. See how you react before adding more.
- Tell your doctor. If you’re taking benzodiazepines, opioids, sleep aids, or muscle relaxers, be honest about cannabis use. They need to adjust doses or find alternatives.
Some patients have successfully reduced opioid use by adding low-dose THC under strict monitoring. But that’s not DIY. It’s done in controlled settings with frequent check-ins and blood tests. Don’t try to replicate that at home.
What’s Changing?
Regulations are catching up. The FDA now requires warning labels on all prescription CNS depressants about cannabis interactions. The European Medicines Agency did the same in 2023. California now requires doctors to complete a 2-hour training on cannabis-depressant risks before certifying patients for medical marijuana. Since that rule started, high-risk combinations dropped by 28%.
Research funding is rising too. The NIH spent $142.7 million in 2023 on cannabis interaction studies-five times more than in 2020. Scientists are now working on risk scores, safe THC thresholds, and whether certain CBD:THC ratios can reduce danger.
But until we have clearer answers, the safest choice is simple: don’t combine them. If you need help managing pain, anxiety, or sleep, talk to your doctor about alternatives that won’t put your life at risk.
Can cannabis and alcohol be safely mixed?
No. Mixing cannabis and alcohol significantly increases dizziness, nausea, impaired coordination, and the risk of vomiting or choking. Both are CNS depressants, and together they can cause extreme sedation, blackouts, and respiratory suppression. Emergency room visits involving both substances have risen sharply since 2019. The safest approach is to avoid combining them entirely.
Is CBD safe to take with benzodiazepines?
High-CBD, low-THC products (like 150 mg CBD with under 0.3% THC) show no significant interaction with benzodiazepines in clinical trials. However, most CBD products sold online or in stores contain unknown levels of THC or other contaminants. Without lab testing and medical oversight, it’s risky. Always consult your doctor before combining CBD with any prescription depressant.
How long does cannabis stay in your system when combined with depressants?
Cannabis metabolites can stay detectable in your body for days or weeks, depending on frequency of use. But the sedative effects-especially when mixed with depressants-peak within hours and can linger for up to 8 hours with edibles. Even after the high fades, your reaction time, memory, and coordination may remain impaired. This is why driving or operating machinery after combining these substances is dangerous, even if you feel fine.
Can cannabis replace my anxiety medication?
Some people report reduced anxiety with low-dose cannabis, but it’s not a reliable or safe substitute for prescribed benzodiazepines or SSRIs. Cannabis can increase anxiety in others, especially at higher THC levels. Abruptly stopping prescribed medication can cause withdrawal. If you want to reduce or stop an anxiety medication, work with your doctor on a supervised taper plan-not self-medication.
What should I do if I accidentally mix cannabis and a depressant?
If you feel extremely drowsy, confused, have trouble breathing, or lose consciousness, call emergency services immediately. Don’t wait. Do not try to sleep it off. Respiratory depression can happen slowly and silently. If you’re with someone who’s unresponsive or breathing very slowly, keep them awake, on their side, and get help right away. Keep a record of what you took and when-this helps medical staff respond faster.
Final Takeaway
Cannabis isn’t inherently dangerous. But when paired with other depressants, it becomes a silent threat. The sedation isn’t just “feeling chill.” It’s your body losing control over basic functions. Millions of people are using these combinations without realizing the risk. The science is clear. The data is real. And the consequences can be fatal. If you’re using cannabis and a CNS depressant, talk to your doctor-not a Reddit thread. Your life isn’t worth gambling on.
13 Comments
Jean Claude de La RondeDecember 11, 2025 AT 05:35
so like... cannabis is just alcohol with better marketing? 🤔 i mean, if you mix it with anything that makes you sleepy, you're basically playing russian roulette with your brainstem. cool. i'll just keep my weed and my wine separate. or not. who even knows anymore.Sylvia FrenzelDecember 11, 2025 AT 16:45
This is why we need stricter regulation. People treat cannabis like it's herbal tea. It's not. It's a pharmacologically active compound that interacts with prescription meds in ways that can kill. The FDA warnings are a start, but they're not enough.Paul DixonDecember 12, 2025 AT 16:43
i used to mix klonopin and edibles for sleep. thought it was my secret weapon. turned out i was just slowly shutting down my breathing. ended up in the er after passing out on the couch. never did it again. thanks for the reminder, this post saved my life.Jimmy KärnfeldtDecember 13, 2025 AT 07:01
i get it. people want relief. pain, anxiety, insomnia-they’re real. but combining substances without knowing how they interact is like driving blindfolded and hoping for the best. i’ve seen friends lose years to this. it’s not about shaming, it’s about awareness. you deserve to feel better without risking your life.Ariel NicholeDecember 14, 2025 AT 16:08
i’ve been on gabapentin for nerve pain and started using low-dose cbd for anxiety. my doc said it’s probably fine but to watch for dizziness. i didn’t realize how common this combo is until i read this. thanks for laying it out clearly.john damonDecember 15, 2025 AT 01:18
just got my 20% gummy and my 5mg oxycodone ready 😌🍷💊 let’s goooooomatthew dendleDecember 16, 2025 AT 13:34
so youre telling me if i smoke and take xanax i might die? shocker. next youll say drinking and driving is bad. maybe dont be an idiot then. this is basic bio 101. why are we even having this conversationTaylor DresslerDecember 17, 2025 AT 00:08
The science here is solid. THC and GABAergics like benzodiazepines both enhance inhibitory neurotransmission-this isn’t theoretical. The risk isn’t just additive; it’s synergistic. That’s why the American Society of Anesthesiologists updated their guidelines. If you’re on any CNS depressant, disclose cannabis use. Full stop. Your doctor isn’t judging you-they’re trying to keep you alive.Aidan StaceyDecember 17, 2025 AT 05:14
i lost my uncle last year. he took a Xanax after a high-THC edible to ‘chill out’. didn’t wake up. no one knew he was using both. the coroner said respiratory depression. this isn’t a myth. it’s happening to real people. please, if you’re doing this, stop. talk to someone. you’re not alone.Jim IrishDecember 19, 2025 AT 01:18
Cannabis affects everyone differently. But the data shows clear patterns. Older adults on multiple medications are especially vulnerable. The body’s ability to metabolize drugs declines with age. Add cannabis, and the margin for error vanishes. Awareness saves lives.Kristi PopeDecember 20, 2025 AT 03:10
i used to think cbd was the magic fix for my anxiety. turned out the little bit of THC in my oil was making me paranoid and foggy. switched to isolate, told my psych, and we adjusted my lexapro. i feel like myself again. it’s not about giving up weed-it’s about choosing wiselyAman deepDecember 21, 2025 AT 03:31
in india we use bhang sometimes with milk during festivals. never heard of anyone having trouble. but here, people mix it with pills like candy. maybe its not the plant, its how we use it. i hope more doctors start asking, not judgingEddie BennettDecember 21, 2025 AT 21:40
i’m not saying don’t use cannabis. i’m saying know your dose, know your meds, and don’t be a hero. i’ve been on 20mg of oxycodone for 5 years. started low-dose cbd for sleep. no issues. but i track everything. i don’t guess. if you’re not tracking, you’re gambling.