When a patient walks into the ER with shortness of breath, the clock starts ticking. Is it heart failure? COPD? A pulmonary embolism? Or just anxiety? In the past, doctors relied on chest X-rays, EKGs, and sometimes invasive tests to find out. Today, one simple blood test can cut through the noise: NT-proBNP.
What NT-proBNP Actually Measures
NT-proBNP stands for N-terminal pro-B-type natriuretic peptide. It’s a protein fragment released by the heart when the ventricles are stretched from too much pressure or fluid. Think of it like your heart screaming for help - this is the chemical version of that scream. Unlike BNP, which breaks down quickly, NT-proBNP stays stable in the blood for hours, making it easier to measure accurately even if there’s a delay in testing.
The test is done with just one vial of blood - no fasting, no special prep. Results come back in under an hour in most hospitals, and the cost is under $20. The Roche Elecsys assay dominates the market, used in over 70% of U.S. labs. It detects levels as low as 5 pg/mL, with a range up to 35,000 pg/mL. That’s critical because the difference between normal and dangerous can be as small as 100 points.
When to Order the Test - The Clear Indications
There are five situations where NT-proBNP isn’t just helpful - it’s essential.
- Suspected acute heart failure - If someone comes in with sudden breathlessness, swelling in the legs, or fatigue, and you’re unsure if it’s cardiac or pulmonary, NT-proBNP is your first step. A level below 300 pg/mL rules out heart failure with 98% confidence. That means you can avoid unnecessary echocardiograms, CT scans, and hospital admissions.
- Emergency department triage - NICE guidelines in the UK and ESC guidelines in Europe both give NT-proBNP a Class I recommendation for all patients presenting with acute dyspnea. In fact, hospitals that use it routinely see a 19% drop in unnecessary echocardiograms, according to the UK National Audit of Heart Failure.
- Assessing chronic heart failure - For patients already diagnosed, NT-proBNP levels track disease progression. Rising levels mean the heart is worsening. Falling levels after treatment suggest the therapy is working. It’s more reliable than symptoms alone.
- Prognosis in acute coronary syndrome - Even if the patient doesn’t have full heart failure, an elevated NT-proBNP after a heart attack predicts higher risk of death or rehospitalization. The 2024 ACC/AHA/HFSA guidelines will soon formalize this use.
- Monitoring high-risk patients - Patients with diabetes, hypertension, or atrial fibrillation are at higher risk for developing heart failure. Checking NT-proBNP annually can catch early signs before symptoms appear.
Age and Comorbidities Change Everything
Here’s where things get tricky. NT-proBNP isn’t a one-size-fits-all number. Levels naturally rise with age - about 15-20% higher per decade - even in perfectly healthy people.
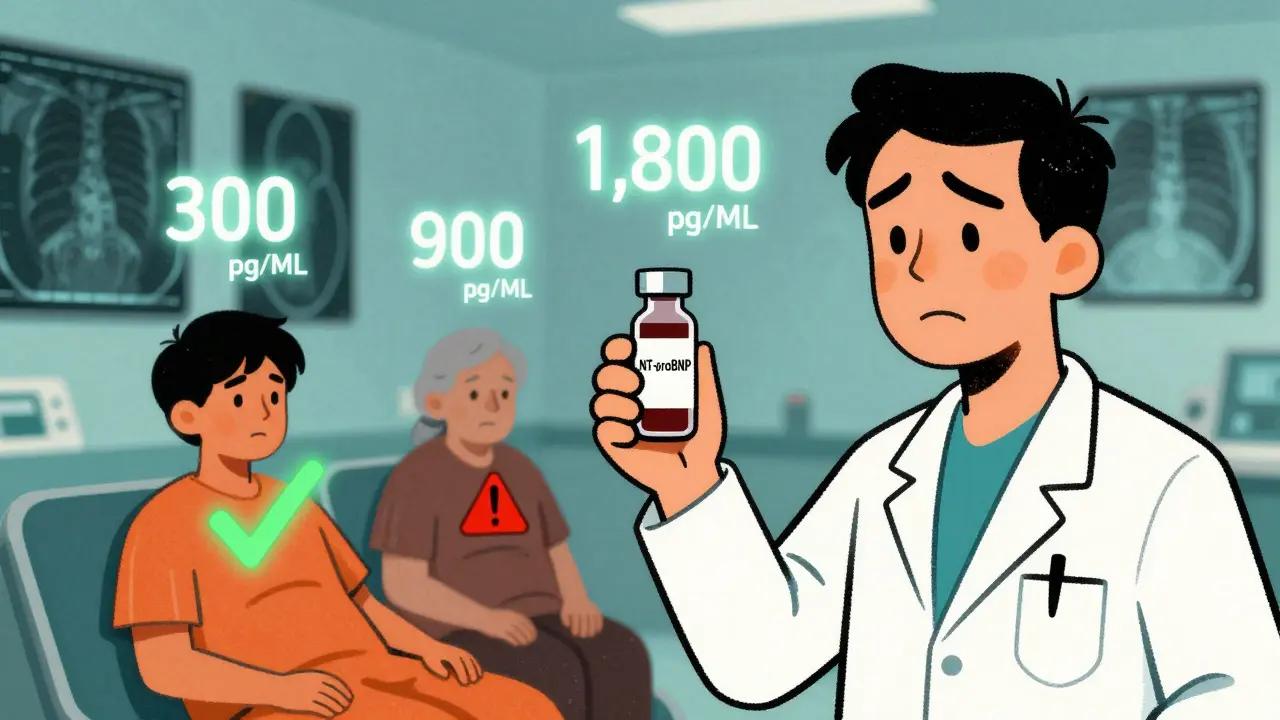
That’s why cutoffs aren’t fixed:
- Under 50 years: rule-out threshold is < 450 pg/mL
- 50-75 years: < 900 pg/mL
- Over 75 years: < 1,800 pg/mL
But it gets more complicated. Kidney disease skews results. In patients with stage 3 or 4 chronic kidney disease (CKD), NT-proBNP levels rise 28-40% without any heart failure. So if a 78-year-old with CKD has a level of 850 pg/mL, is that heart failure or just bad kidneys? The answer: you can’t tell from the number alone. In these cases, use the modified ESC cutoff of <1,200 pg/mL to rule out heart failure.
Obesity does the opposite. For every 5-point increase in BMI, NT-proBNP drops 25-30%. So a 60-year-old obese patient with a level of 200 pg/mL might still have heart failure - the test is under-reporting the problem. Never rely on a low number if clinical signs point strongly to heart failure.

Why NT-proBNP Beats BNP
You might wonder: why not just use BNP? Both are natriuretic peptides, but NT-proBNP has clear advantages:
| Feature | NT-proBNP | BNP |
|---|---|---|
| Half-life | 60-120 minutes | 20 minutes |
| Stability in sample | 72 hours at 4°C | 4 hours at room temp |
| Diagnostic accuracy (AUC) | 0.91 | 0.88 |
| Renal clearance | Higher - needs adjustment in CKD | Lower |
| Market share (U.S.) | 68% | 32% |
The longer half-life means NT-proBNP is less affected by delays in processing. A sample sitting in the lab for two hours? No problem. BNP would degrade. That’s why 92% of hospitals now prefer NT-proBNP, and why it’s the default in most emergency protocols.
What the Test Won’t Tell You
NT-proBNP is powerful - but it’s not magic. It doesn’t tell you the cause of heart failure. It won’t show you if there’s a valve problem, a blocked artery, or a rhythm disorder. It doesn’t replace echocardiography, physical exam, or patient history.
And it can’t be used alone in asymptomatic patients. Medicare data shows 18% of NT-proBNP tests are ordered on people with no symptoms - like those with just high blood pressure or a family history. That’s overuse. Starting January 2025, Medicare will require prior authorization for testing in low-risk, asymptomatic patients to curb unnecessary costs.
Dr. Allan Jaffe from Mayo Clinic puts it bluntly: “NT-proBNP should never be used in isolation.” A level of 1,500 pg/mL in a 70-year-old with atrial fibrillation and mild kidney disease? That’s a red flag - but not a diagnosis. You need to look at the whole picture.
Real-World Impact: Stories from the Front Lines
Cardiologists report dramatic changes since adopting NT-proBNP routinely.
Dr. Sarah Chen, a hospitalist in Ohio, shared on Reddit: “NT-proBNP saved me from ordering a $3,000 echocardiogram for an 82-year-old with COPD. Her level was 120 pg/mL. Turned out to be a severe asthma flare - no heart failure. We treated her with steroids and sent her home the same day.”
Another case: a 69-year-old man with fatigue and swollen ankles. His doctor ordered a chest X-ray, which showed mild congestion. But the NT-proBNP came back at 1,750 pg/mL. That’s high for his age. He was referred for echo, which revealed severe left ventricular dysfunction. He started on guideline-directed therapy and avoided hospitalization.
But the frustration is real too. Dr. Michael Rodriguez wrote on the American College of Physicians forum: “I had a patient with NT-proBNP at 850 pg/mL - 78, AFib, CKD stage 3. Is this heart failure? Or just aging and kidney disease? There’s no clear answer. That’s the gray zone.”
That’s why the Heart Failure Society of America runs a free NT-proBNP Interpretation Hotline (1-800-NT-PROBNP). They get 1,200 calls a month. Clinicians call when they’re stuck - and 94% say the advice helped them make the right call.
What’s Next for NT-proBNP?
The future is faster and more accessible. In 2023, the FDA cleared Roche’s Cobas h 232 - a point-of-care device that gives NT-proBNP results in 12 minutes. It’s now being rolled out in urgent care centers and ambulances. Imagine a paramedic running the test in the field and knowing whether to take the patient to a heart failure center or a pulmonary unit.
Research is also expanding its use. The VICTORIA trial showed that a drop in NT-proBNP after treatment for heart failure predicted a 35% lower risk of death. That means the test may soon be used to guide therapy - not just diagnose it.
Despite new multi-marker panels on the horizon, NT-proBNP remains unmatched. With 28 years of outcome data backing it, it’s not going anywhere. Evaluate MedTech projects it will remain the gold standard through 2030.
Bottom Line: When to Order
Don’t order NT-proBNP for every patient with a cough. But if someone has:
- Sudden shortness of breath
- Unexplained fatigue or swelling
- Known heart disease with new symptoms
- High-risk conditions (diabetes, CKD, AFib) with worsening function
- then order it. It’s fast, cheap, and saves lives by avoiding false leads and unnecessary tests. Use age- and kidney-adjusted cutoffs. Never ignore the clinical picture. And when in doubt? Call the hotline.
NT-proBNP isn’t just a lab result. It’s a decision-making tool. Used right, it turns uncertainty into clarity - in minutes, with one drop of blood.
What is a normal NT-proBNP level?
There’s no single normal level - it depends on age. Under 50, under 450 pg/mL is normal. Between 50 and 75, under 900 pg/mL. Over 75, under 1,800 pg/mL. Levels above these thresholds raise suspicion for heart failure, but they must be interpreted with clinical context.
Can NT-proBNP be used to diagnose heart failure in obese patients?
Yes, but it’s less reliable. Obesity lowers NT-proBNP levels by 25-30% for every 5-point increase in BMI. So a low level in an obese patient doesn’t rule out heart failure. Always correlate with symptoms, physical exam, and imaging. Don’t rely on the number alone.
Does kidney disease affect NT-proBNP results?
Yes. In chronic kidney disease stages 3-5, NT-proBNP levels rise 28-40% even without heart failure. Use a higher rule-out cutoff of <1,200 pg/mL in these patients. Never assume an elevated level means heart failure - it could be kidney-related.
Is NT-proBNP better than BNP for heart failure testing?
Yes, for most clinical settings. NT-proBNP is more stable, has a longer half-life, and shows slightly better diagnostic accuracy (AUC 0.91 vs. 0.88). It’s the preferred test in 68% of U.S. labs. BNP is still used, but NT-proBNP is now the standard in guidelines and emergency protocols.
Can NT-proBNP predict heart failure before symptoms appear?
In high-risk patients - like those with diabetes, hypertension, or atrial fibrillation - rising NT-proBNP levels can signal early heart strain before symptoms develop. Annual screening isn’t routine yet, but emerging data supports its use for early intervention. Always pair it with clinical evaluation.
Why is Medicare requiring prior authorization for NT-proBNP tests now?
Because 18% of tests were being ordered on asymptomatic patients with no clear indication - like routine checkups for people with just high blood pressure. This was driving up costs without improving outcomes. Starting January 2025, prior authorization is required to ensure the test is only used when clinically justified.
Next Steps for Clinicians
If you’re not using NT-proBNP routinely, start now. Keep the age-adjusted cutoffs handy. Print them. Put them on your EHR template. Train your staff on when to order it - and when not to.
If you’re already using it, don’t fall into the trap of over-reliance. Always ask: What’s the clinical story? Is the patient obese? Do they have kidney disease? Are they on diuretics? The number is a clue - not a verdict.
And if you’re unsure? Call the Heart Failure Society hotline. It’s free, it’s real, and it’s used by thousands of clinicians every month. That’s how you turn a lab result into a better decision.
14 Comments
Akshaya Gandra _ Student - EastCaryMSJanuary 4, 2026 AT 12:05
so like... if my grandma has kidney issues and her nt-probnp is 800, does that mean she's dying or just needs more water?? i'm so confused lol
Cassie TynanJanuary 4, 2026 AT 16:01
oh great. another blood test that costs less than my latte but somehow makes doctors feel like wizards. next they'll tell us to check our soul's BNP levels.
Rory CorriganJanuary 5, 2026 AT 00:07
heart screaming for help... 🤔
so if my heart yells 'I'M OVERWORKED' and the test picks it up... why don't we just ask it nicely to chill out first? 😅
Stephen CraigJanuary 6, 2026 AT 16:10
NT-proBNP is the most underused tool in emergency medicine. It’s not perfect, but it’s the closest thing we have to a clinical crystal ball.
Connor HaleJanuary 8, 2026 AT 02:56
the fact that a single vial of blood can prevent a dozen unnecessary scans is wild. medicine is getting weirdly efficient. i kinda like it.
Charlotte NJanuary 9, 2026 AT 01:40
wait so if you're over 75 and have CKD and your level is 1750... is that normal?? or is it heart failure?? or is it both?? or is it just... aging?? i need a flowchart
bob bobJanuary 9, 2026 AT 03:36
my uncle got admitted for 'shortness of breath' and they did this test and he was fine. saved him a week in the hospital and a bunch of stress. this test is a gift.
Uzoamaka NwankpaJanuary 10, 2026 AT 23:57
they say it's a simple test but what if the lab messes up? what if the machine is broken? what if someone's blood is just... weird? what if this is all part of a pharmaceutical plot to sell more drugs??
Siobhan GogginJanuary 11, 2026 AT 10:41
finally! a test that actually helps instead of just adding to the bill. i wish we had this when my mum was sick. thank you science.
Vikram SujayJanuary 11, 2026 AT 21:44
While the utility of NT-proBNP in clinical decision-making is empirically supported, one must remain cognizant of the confounding variables inherent in geriatric and nephropathic populations. Standardization remains a challenge.
Jay TejadaJanuary 13, 2026 AT 04:23
yeah but like... if you're 80 and your kidneys are done and your heart is tired... who even cares anymore? just give 'em soup and a blanket.
Shanna SungJanuary 13, 2026 AT 17:41
they're hiding the real truth-this test was invented to make you buy more meds. the FDA is in bed with Roche. they don't want you to know you can fix heart failure with turmeric and yoga
Mandy KowitzJanuary 14, 2026 AT 19:19
so you're telling me we're paying doctors to read a number instead of actually talking to patients? genius. let's just replace all ERs with a QR code.
Michael RudgeJanuary 16, 2026 AT 12:57
It's fascinating how the medical community has elevated a simple biomarker to the status of oracle. Meanwhile, we still can't diagnose anxiety without a 45-minute questionnaire and a $200 copay. The hypocrisy is breathtaking.