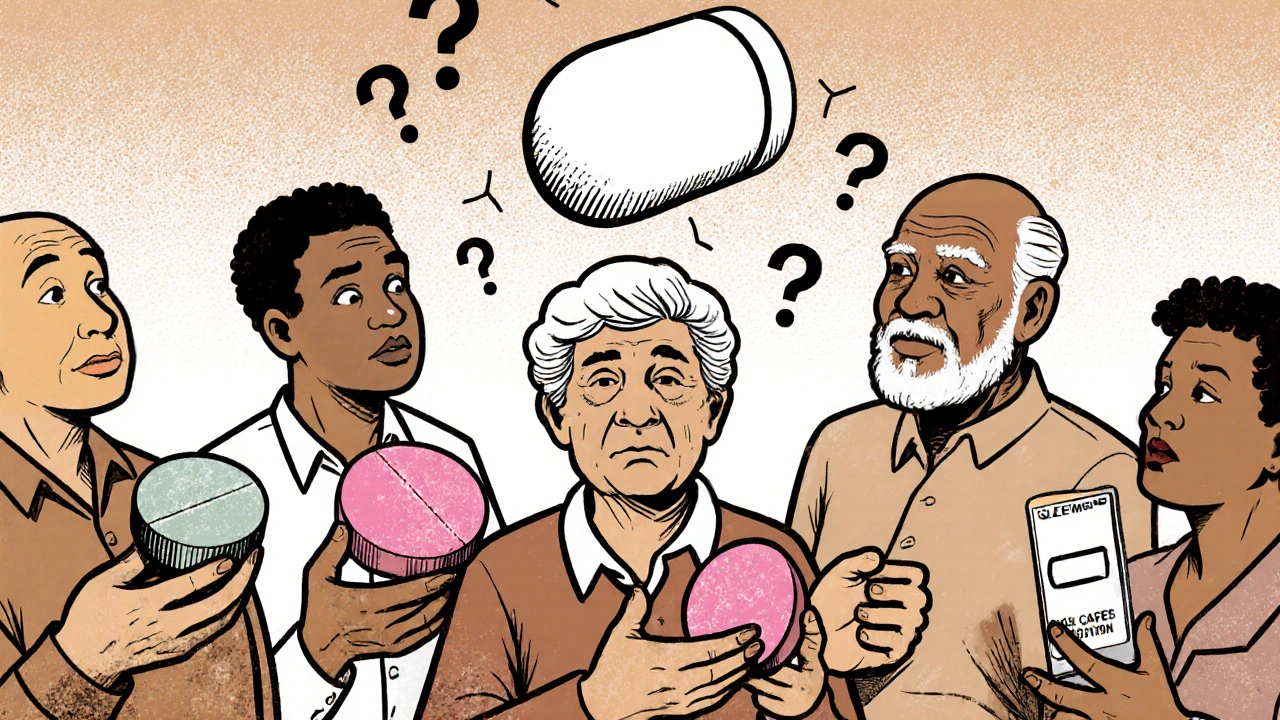
Every year, millions of people in the U.S. switch from brand-name drugs to generics to save money. But here’s the problem: many don’t understand what generics are, or why their pills look different now. This isn’t just about cost-it’s about safety. When patients don’t recognize their medication because it changed shape, color, or label, they might skip doses, take too much, or stop altogether. And the consequences? Hospital visits, worsening conditions, and higher healthcare costs.
Why Generic Medications Confuse Patients
Generic drugs are chemically identical to brand-name versions. They contain the same active ingredient, work the same way, and meet the same FDA standards. But they don’t look the same. A pill that was once a white oval might become a pink round tablet. The packaging changes. The name on the bottle might say something completely different. This isn’t random. Generic manufacturers are allowed to make their versions look different. And that’s where things go wrong. A 2016 study found that 42% of patients didn’t know generics are just as effective as brand-name drugs. Older adults, people with low health literacy, and those managing multiple medications are hit hardest. One woman with type 2 diabetes stopped taking her metformin for three days because the new pills looked nothing like the old ones. She ended up in the ER with dangerously high blood sugar. It’s not just about looks. Patients often think, “If it doesn’t look the same, it must be different.” That belief is reinforced by the fact that brand-name drugs are advertised heavily. You see commercials, logos, and catchy names. Generics? They’re silent. No ads. No recognition. Just a plain label and a lower price.The Real Cost of Confusion
Medication errors tied to generic confusion aren’t rare. Between 2015 and 2020, over 1,200 medication errors were reported because patients mixed up different versions of the same generic drug. That’s 17% of all generic-related errors. And it’s not just accidents-it’s intentional avoidance. A 2020 Kaiser Family Foundation analysis found that Medicare patients with low health literacy were 3.1 times more likely to refuse a generic substitution, even when their doctor recommended it. Older adults are especially vulnerable. A 2021 study in the Journal of the American Geriatrics Society found that 52% of seniors taking heart medications admitted to “pill dumping”-throwing away pills that looked unfamiliar. One man with high blood pressure tossed his new generic lisinopril because it was blue instead of white. He didn’t call his doctor. He just assumed it wasn’t right. And the ripple effect is real. When patients don’t take their meds as prescribed, their conditions worsen. Diabetes, hypertension, and depression get harder to control. Emergency room visits go up. Costs climb. The CDC estimates that poor medication adherence adds $300 billion annually to U.S. healthcare spending.What Makes Health Literacy So Hard with Generics
Health literacy isn’t just about reading ability. It’s about understanding instructions, recognizing changes, remembering names, and knowing when to ask questions. The National Network of Libraries of Medicine says 80 million American adults have basic or below-basic health literacy. That means they struggle with terms like “active ingredient,” “therapeutic equivalence,” or even “generic.” The problem is compounded by how information is delivered. Most generic drug leaflets are written in dense, legal-speak. A 2022 FDA review found only 37% of generic manufacturers used plain language. Instructions like “take once daily with food” might be buried in small print. Side effects are listed in medical jargon. And nowhere does it say: “This is the same medicine you’ve taken before, just made by a different company.” Even doctors and pharmacists aren’t always equipped to explain it. A 2022 American Medical Association report said 56% of physicians hear patients express confusion about generic substitutions during visits. Many providers assume patients understand because they’ve been told before. But without checking for understanding, the message gets lost.
What Works: Real Solutions That Reduce Confusion
The good news? We know what helps. And it’s not complicated. The Ask Me 3 program trains healthcare providers to ask three simple questions:- What is my main problem?
- What do I need to do?
- Why is it important?
What’s Changing on the Policy Side
Governments and agencies are finally paying attention. The FDA’s 2023 draft guidance proposes standardized color-coding for therapeutic classes. For example, all blood pressure meds could be blue, all diabetes pills yellow. This idea comes from Australia, where color-coding cut medication errors by 33%. The European Union already requires standardized packaging for generics in many countries-and saw a 27% drop in errors. The Biden administration’s 2023 National Action Plan to Improve Health Literacy includes a specific goal: reduce generic medication confusion-related errors by 25% by 2027. The WHO’s 2023 Global Health Literacy Action Plan lists generic standardization as a top priority, with pilot programs in 15 low- and middle-income countries showing a 41% improvement in correct medication use when visuals were consistent. Pharmacists are also stepping up. The American Pharmacists Association now recommends that pharmacists assess a patient’s understanding before switching to a generic. As of October 2023, 38 states have introduced legislation supporting this practice.What You Can Do Right Now
If you or someone you care about takes generics, here’s what to do:- Ask: “Is this the same medicine I was taking before?”
- Check: Compare the old pill and the new one. Note the shape, color, and imprint (the letters or numbers on the pill).
- Take a photo: Keep a picture of each pill on your phone. When it changes, you’ll know right away.
- Use an app: Try Medisafe or another pill tracker that lets you scan and store your meds.
- Bring all your pills to every doctor visit-even the ones you think you don’t take anymore.
- Don’t assume: If it looks different, don’t guess. Call your pharmacist. They’re paid to explain this stuff.
The Bigger Picture
This isn’t just about pills. It’s about dignity. It’s about trust. When patients feel confused or dismissed, they stop engaging with their own care. And that’s when health systems fail. The solution isn’t more pamphlets. It’s not just better labeling. It’s changing how we talk about medicine. We need to treat health literacy like a design problem-not a patient problem. If a pill’s appearance changes, the system should adapt, not the person. The tools, the research, the policies-all of it exists. What’s missing is consistent action. Every time a pharmacist explains a generic switch clearly. Every time a doctor checks for understanding. Every time a patient feels heard. That’s how we stop the confusion before it starts.Generic medications save billions. But they only work if people know how to use them.
Are generic drugs really the same as brand-name drugs?
Yes. Generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. The FDA requires them to be bioequivalent, meaning they work the same way in the body. The only differences are in inactive ingredients (like fillers or dyes), shape, color, and packaging-all of which don’t affect how the drug works.
Why do generic pills look different every time I refill them?
Different manufacturers make the same generic drug. Each one chooses its own color, shape, and imprint to distinguish its product. This is allowed by law, but it causes confusion. A pill you’ve taken for years might suddenly look completely different. That’s why it’s important to check with your pharmacist when your medication looks new-even if the name is the same.
What should I do if my generic medication looks different?
Don’t stop taking it. Don’t assume it’s wrong. Call your pharmacist and ask: “Is this the same medicine I was taking before?” Show them the old and new pills. Most pharmacists can confirm it’s the same drug and explain the change. You can also use a pill identifier app or check the imprint code online at the FDA’s database.
Can generic drugs be less effective?
No. Generic drugs must meet the same strict standards as brand-name drugs for safety, strength, purity, and performance. The FDA tests them before approval. Studies show no difference in effectiveness between generics and brand-name drugs for most conditions. If you feel a difference, it may be due to inactive ingredients (like dyes or fillers) affecting how your body reacts, not the active drug itself. Talk to your doctor or pharmacist before switching back.
How can I avoid confusion with my medications?
Keep a list of all your medications with their names, doses, and what they’re for. Take a photo of each pill when you first get it. Use a pill tracker app like Medisafe that lets you scan and store your meds. Bring all your bottles to every doctor visit. Ask your pharmacist to explain any changes in appearance. And never assume-always confirm.
Is there help available if I don’t understand my medication instructions?
Yes. Many pharmacies offer free counseling when you pick up a new prescription. Federally Qualified Health Centers and community clinics provide health literacy support. The CDC’s Universal Precautions approach ensures providers explain meds in plain language. You can also ask for printed materials in large print or audio formats. Don’t be afraid to say, “I need this explained again.”
Health literacy isn’t about how smart you are. It’s about how well the system helps you understand. When it comes to generics, clarity saves lives.
10 Comments
Ross RuprechtNovember 21, 2025 AT 21:46
Ugh another one of these posts. I get it, generics are the same. But why do I have to Google my pills every time I refill? My grandma almost took someone else's blood pressure med because the color changed. This isn't rocket science.
Bryson CarrollNovember 23, 2025 AT 00:39
Let's be real here the entire system is designed to confuse people so corporations can keep profiting off brand names while pushing generics that look nothing like the originals. The FDA doesn't care as long as the active ingredient matches. Who cares if your 78-year-old aunt thinks she's getting scammed because her pill is now pink instead of white. Capitalism at its finest.
Lisa LeeNovember 24, 2025 AT 02:55
Why does America even allow this? In Canada the generics have to look almost identical unless there's a medical reason. We don't let people die because they're too lazy to read the label. This is a systemic failure and frankly embarrassing.
Jennifer ShannonNovember 25, 2025 AT 18:40
You know what's fascinating? It's not just about the pills-it's about how we've built a healthcare system that treats patients like puzzles to be solved rather than humans to be supported. We expect people to memorize pill shapes, cross-reference databases, and decode legal jargon just to stay alive. Meanwhile, the system that's supposed to protect them doesn't even bother to standardize colors or add simple icons. It's not laziness, it's design failure. And honestly? It's heartbreaking. I've seen elderly neighbors throw out their meds because they looked 'wrong'-and they didn't feel safe asking because they thought they 'should know.' We need empathy, not apps.
Suzan WanjiruNovember 26, 2025 AT 17:56
My pharmacy started doing brown bag reviews last year and it changed everything. I bring all my meds every time even if nothing changed. They check for interactions, expired stuff, and yes-generic switches. No more guessing. Just ask. Seriously. Just ask. Your pharmacist gets paid to answer this stuff. No shame.
Kezia Katherine LewisNovember 27, 2025 AT 09:46
Therapeutic equivalence is a regulatory construct, not a perceptual one. The bioequivalence parameters established under 21 CFR 320.24 are statistically robust, yet cognitive dissonance persists due to visual incongruence. Patients anchor to perceptual familiarity as a proxy for efficacy-a well-documented heuristic bias. Standardization of pill aesthetics could mitigate this, but regulatory inertia and manufacturer autonomy remain structural barriers.
Javier RainNovember 29, 2025 AT 06:45
STOP waiting for the system to fix itself. Grab your phone. Take a picture of every pill the first time you get it. Save it. When it changes? Pull up the pic. Call your pharmacist. Boom. Done. You're in control now. This isn't hard. It's just inconvenient for people who think healthcare should be easy. It's not. But YOU can make it easier.
Pramod KumarDecember 1, 2025 AT 04:10
Back home in India, we call these 'copy pills'-and everyone knows they're the same. But here? People act like the color change means it's magic or poison. I told my cousin: 'If your sugar pill was white and now it's green, it's still sugar. The label says metformin, right? Then it works.' He laughed and said he never thought of it that way. Sometimes all you need is someone to say it simple.
Katy BellDecember 2, 2025 AT 10:09
I cried reading this. My mom took her heart meds for 12 years. Then one day the pill turned from white to pale yellow. She didn't say anything for three weeks. She just stopped taking them. Said she didn't trust it. When I found out, I had to drive 90 minutes to sit with her while she called the pharmacist. She was so ashamed. She thought she was dumb. She's not dumb. The system is broken.
Ragini SharmaDecember 3, 2025 AT 18:03
wait so u mean to tell me that my blue pill that looks like a tiny space rock is the same as my old white one? lol i thought they swapped it for a new drug 😂 i just googled the imprint and it was the same. soooo yeah. also i used medisafe and it saved my life. or at least my sanity.