TCA Blood Level Checker
TCA Blood Level Assessment
Check if your TCA blood level is safe, in warning zone, or toxic based on clinical guidelines. Results are based on trough-level testing (blood drawn right before next dose).
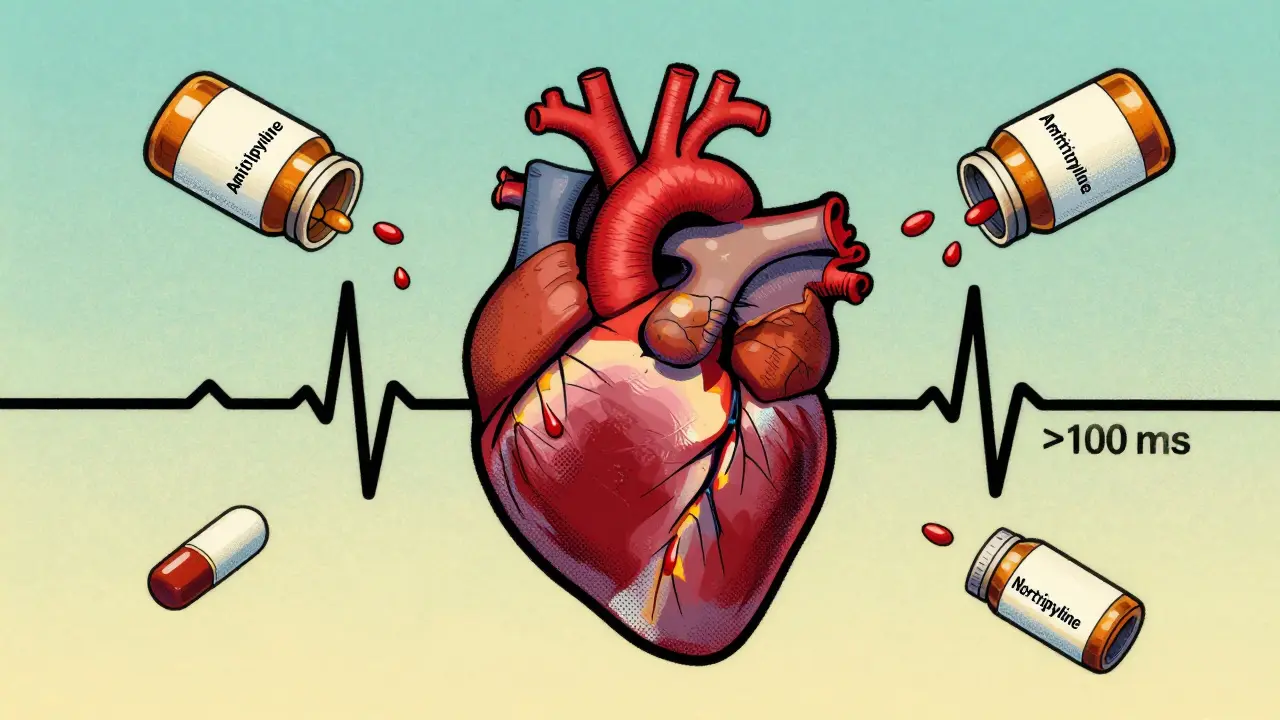
Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline aren’t used as often as they once were. But for some people - especially those with treatment-resistant depression or chronic nerve pain - they’re still the best option. The problem? These drugs are dangerously close to being toxic. A single extra pill can send someone to the ICU. That’s why therapeutic drug monitoring (TDM) isn’t optional. It’s life-saving.
Why TCAs Are So Risky
TCAs work by boosting serotonin and norepinephrine in the brain. But they don’t stop there. They also block receptors all over the body: heart muscle, saliva glands, intestines, even the brain’s electrical signals. That’s why side effects like dry mouth, constipation, and drowsiness are common. But when levels creep too high, things turn deadly.At blood levels above 500 ng/mL, TCAs can cause:
- QRS widening on ECG (>100 ms) - this means the heart’s electrical signal is slowing down dangerously
- QT prolongation - which can trigger a chaotic heart rhythm called torsades de pointes
- Seizures
- Coma or respiratory arrest
Here’s the scary part: some people die from just one extra dose. The Royal Children’s Hospital in Melbourne documented cases where a single tablet overdose killed adults with no history of suicide. Even patients taking their prescribed dose can slip into toxicity if their body metabolizes the drug too slowly - and that’s where TDM comes in.
What Therapeutic Drug Monitoring Actually Measures
TDM isn’t just checking if you’re taking your pills. It’s measuring exactly how much drug is in your blood. For TCAs, that means tracking both the original drug and its active breakdown products.Here are the accepted therapeutic ranges:
| Drug | Therapeutic Range (ng/mL) | Toxic Threshold (ng/mL) |
|---|---|---|
| Amitriptyline | 80-200 | >500 |
| Nortriptyline | 50-150 | >300 |
| Desipramine | 100-300 | >400 |
These numbers aren’t guesses. They’re based on decades of clinical data. Levels below 80 ng/mL often mean the drug isn’t working. Levels above 200 ng/mL for amitriptyline? That’s a red flag - even if the patient feels fine.
But here’s the catch: the test isn’t useful unless it’s done right. Blood must be drawn right before the next dose - called the trough level. Why? Because that’s when the drug concentration is most stable. If you draw blood too soon after taking the pill, you’ll get a false high reading. And you need to wait at least 5-7 days after starting or changing the dose. That’s how long it takes for the drug to reach steady state in your body.
Who Needs TDM the Most
Not everyone on TCAs needs regular blood tests. But some groups are at much higher risk:- Elderly patients - 40% of all TCA users are over 65. Their liver and kidneys don’t clear drugs as well. They’re also more sensitive to anticholinergic effects like confusion and urinary retention.
- People with heart disease - even mild QRS prolongation can be dangerous if you’ve had a prior heart attack.
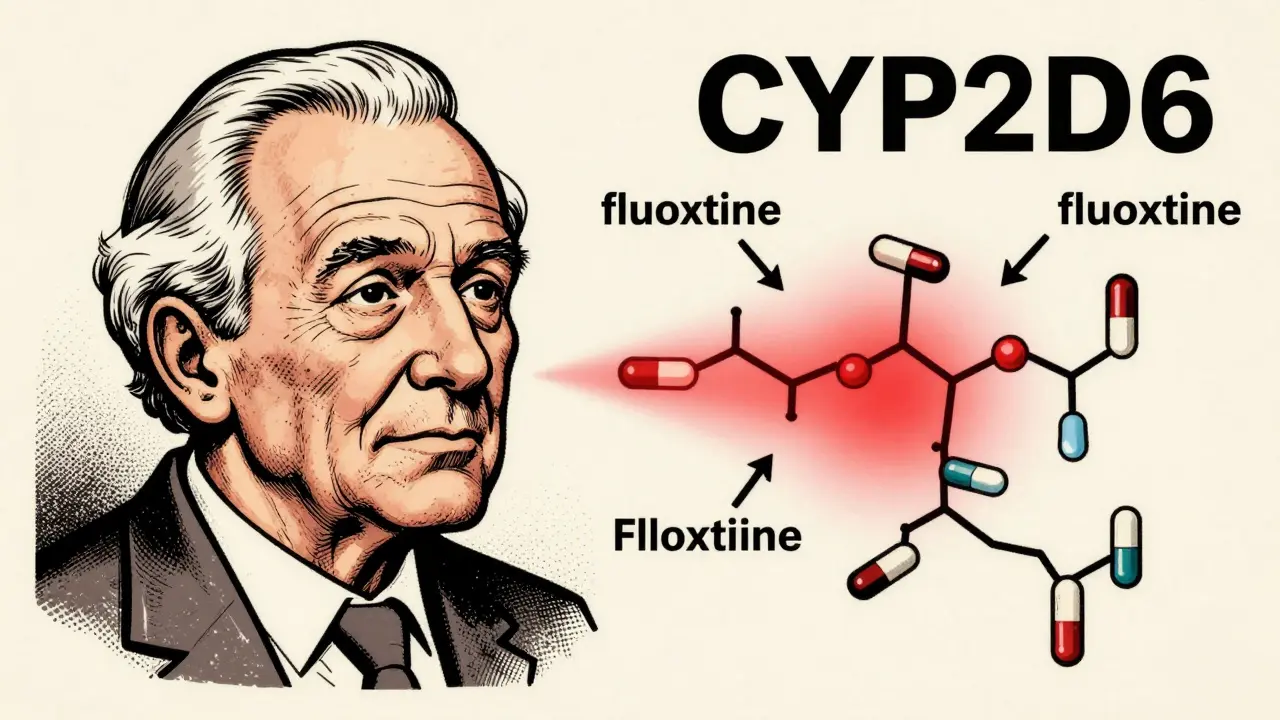
- Those on multiple medications - drugs like fluoxetine, bupropion, or even some antibiotics can block the enzyme (CYP2D6) that breaks down TCAs. This can cause levels to spike 3-5 times higher than expected.
- People with genetic differences - about 7% of people are poor metabolizers of CYP2D6. They process TCAs so slowly that normal doses become toxic. Others are ultrarapid metabolizers - they clear the drug so fast it doesn’t work at all.
At Johns Hopkins, a 78-year-old woman was on 150 mg of nortriptyline daily. Her levels hit 185 ng/mL - above the 150 ng/mL safety limit. She had no symptoms. No dizziness. No confusion. But her ECG showed early QRS widening. Her doctor cut the dose in half. Two weeks later, her level dropped to 120 ng/mL. No more ECG changes. She stayed out of the hospital.
The Hidden Flaws in TDM
TDM sounds simple. But in real life, it’s messy.Most labs take 24-48 hours to return results. That’s too long if someone’s getting worse. A study across 12 European hospitals found that 37.5% of TDM requests were missing key info - like what other drugs the patient was taking. Without that, doctors can’t tell if the high level is from overdose… or from a drug interaction.
And here’s the kicker: 25-40% of TDM requests are filled out poorly. Some doctors don’t even note the time of the last dose. Others order the test after just three days - way too early. The result? Doctors make wrong dose adjustments. A 2023 study found that 20% of TCA dose changes were based on misinterpreted TDM results.
Even worse - some labs use different reference ranges. One lab says 80-200 ng/mL is normal for amitriptyline. Another says 70-190. That 10-15% variation can mean the difference between a safe dose and a dangerous one.
When TDM Fails - And When It Saves Lives
There’s no perfect test. A 42-year-old woman in a 2016 case study had amitriptyline levels at 190 ng/mL - right in the therapeutic range. But her ECG showed QRS widening to 140 ms. She had a seizure. Why? She was unusually sensitive. Her brain and heart reacted to lower levels than most people.That’s why TDM alone isn’t enough. You must always combine blood levels with clinical signs. If someone has a fast heart rate, dry mouth, confusion, or a widened QRS - even if the level is "normal" - treat it like toxicity. Don’t wait for the lab.
On the flip side, proactive TDM prevents disasters. One psychiatrist in Ohio told Reddit users he’d prevented three ICU admissions in a single year just by checking TCA levels before patients felt bad. He didn’t wait for symptoms. He didn’t wait for the patient to say they felt "off." He tested every 6-8 weeks in older patients. That’s the difference between a routine check-up and a life saved.

What’s Changing Now
TCAs aren’t going away. Even though prescriptions dropped from 23 million in 2000 to just 5 million in 2022, they’re still the go-to for nerve pain and treatment-resistant depression in older adults.New tools are making TDM smarter:
- Point-of-care devices - Siemens Healthineers just launched a handheld device in Europe that gives TCA results in 20 minutes. No more waiting two days.
- AI prediction tools - The FDA cleared a system called PsychX Analytics that combines TDM data, ECG readings, and patient symptoms to predict toxicity risk. It’s not perfect, but it flags high-risk cases faster.
- Genetic testing - More clinics now test for CYP2D6 and CYP2C19 genes before prescribing TCAs. If you’re a poor metabolizer, you start on half the usual dose. That cuts the need for follow-up TDM by 40%.
The future? Continuous monitoring - like a glucose sensor for antidepressants. Early trials show that interstitial fluid levels match serum levels 92% of the time. If this works, we might one day see TCAs monitored like insulin in diabetes.
Bottom Line: TDM Isn’t Optional - It’s Essential
TCAs are powerful. But they’re also fragile. A tiny dose change, a new medication, or a genetic quirk can turn a helpful drug into a deadly one. Clinical judgment alone isn’t enough. You need the numbers.For elderly patients, those on multiple drugs, or anyone with heart issues - TDM isn’t a luxury. It’s the only way to know if the dose is safe. And for prescribers? If you’re not ordering TDM for your TCA patients, you’re gambling with their lives.
The data is clear: when TDM is done right, hospitalizations drop by 35%. Deaths from TCA toxicity are rare - but they still happen. And almost every one of them could have been prevented.
How often should TCA blood levels be checked?
The first test should be done after 5-7 days of consistent dosing to reach steady state. After that, check every 6-12 weeks in stable patients. More frequent testing is needed if the dose changes, if new medications are added, or if the patient is elderly or has kidney/liver problems.
Can you overdose on TCAs even if you’re taking them as prescribed?
Yes. Many overdoses aren’t intentional. A patient might accidentally take two pills, or a drug interaction (like with fluoxetine) can cause levels to spike. Genetic differences also play a role - some people naturally process TCAs much slower than others. That’s why TDM is critical even for "perfect" adherence.
Is TDM covered by insurance?
In the U.S., most insurance plans cover TDM for TCAs when medically necessary. The cost ranges from $150 to $250 per test. In the UK and EU, it’s often covered under public health systems. However, some insurers require prior authorization or proof of clinical need - like abnormal ECG findings or side effects.
Why not just use SSRIs instead?
SSRIs are safer in overdose and have fewer side effects - which is why they’re first-line. But they don’t work for everyone. About 30% of people with depression don’t respond to SSRIs. TCAs remain one of the most effective options for treatment-resistant cases. They’re also superior for certain types of nerve pain, like diabetic neuropathy or post-herpetic neuralgia.
What should you do if you suspect TCA toxicity?
Don’t wait for blood test results. If someone has a widened QRS (>100 ms), seizures, confusion, or a fast irregular heartbeat, treat immediately. Administer sodium bicarbonate IV to correct heart rhythm, provide oxygen, and monitor in a hospital. TDM helps prevent toxicity - but it doesn’t replace emergency care when toxicity is already happening.