For people with type 2 diabetes, managing blood sugar isn't just about counting carbs or taking insulin anymore. A new class of medications called SGLT2 inhibitors has changed the game-not just for blood sugar, but for the heart and kidneys too. These drugs, including Jardiance, Farxiga, Invokana, and Steglatro, were originally designed to lower glucose. But what they’ve turned out to do goes far beyond that. They reduce hospital stays for heart failure, slow kidney damage, and even lower the risk of dying from heart-related causes. And yet, they come with real risks: infections, dehydration, and rare but dangerous conditions like diabetic ketoacidosis. If you’re considering or already taking one of these drugs, you need to know both sides.
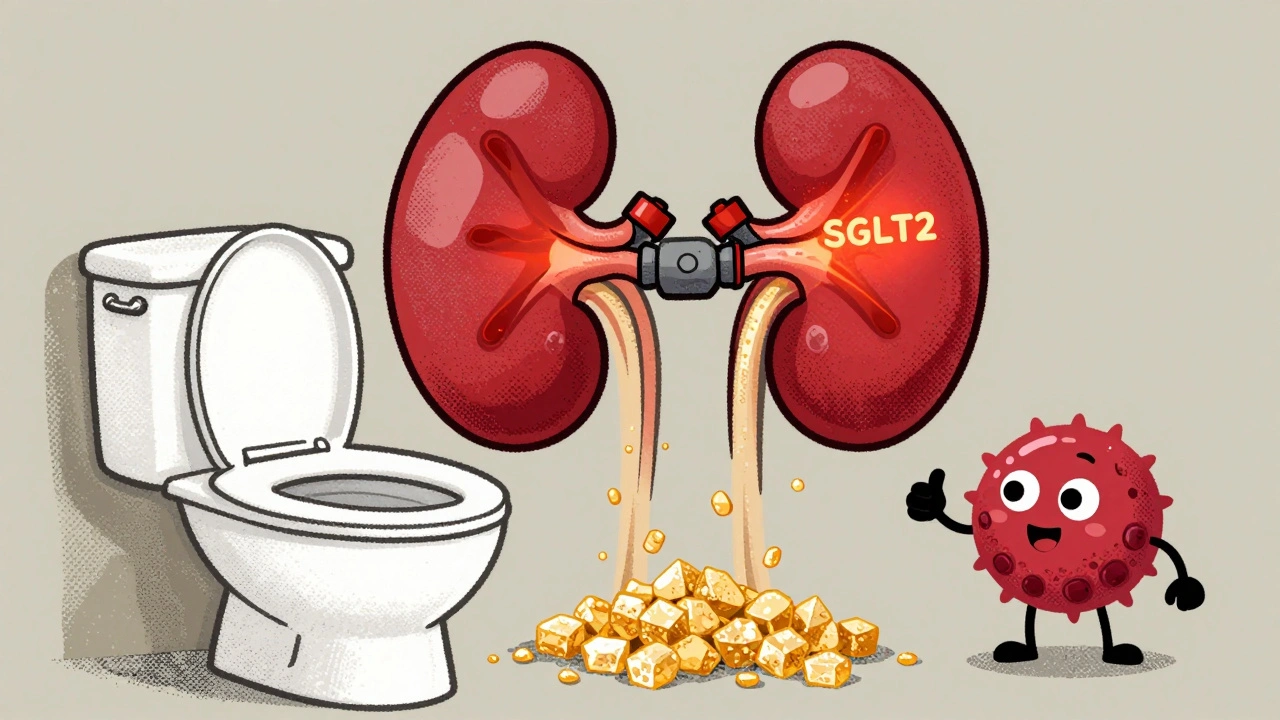
How SGLT2 Inhibitors Actually Work
Unlike most diabetes meds that push insulin or block sugar production, SGLT2 inhibitors work in the kidneys. They block a protein called SGLT2, which normally reabsorbs glucose back into the blood from urine. When this protein is turned off, excess sugar gets flushed out through the pee-about 40 to 100 grams a day. That’s like dumping two to five sugar packets into the toilet every day. The result? Blood sugar drops by 0.5% to 1% on HbA1c, without causing dangerous low blood sugar episodes. This makes them safer than sulfonylureas or insulin for many patients.
Because they’re excreting sugar, these drugs also cause a small amount of weight loss-usually 2 to 3 kilograms over a few months. Blood pressure drops too, by about 3 to 5 mmHg, just from the extra fluid loss. That’s why they’re now recommended not just for diabetes, but for heart and kidney protection, even in people without diabetes.
The Big Benefits: Heart and Kidneys First
The biggest shift in how doctors use SGLT2 inhibitors happened after large clinical trials proved they save lives. The EMPA-REG OUTCOME trial showed empagliflozin reduced cardiovascular death by 38% in patients with existing heart disease. The CREDENCE trial found canagliflozin cut the risk of kidney failure, dialysis, or death from kidney disease by 30%. These weren’t small effects-they were game-changers.
Now, the American Diabetes Association says if you have type 2 diabetes and heart failure, chronic kidney disease, or a history of heart attack, you should start an SGLT2 inhibitor right away-even before metformin in some cases. That’s a massive change from just a decade ago, when these drugs were last-resort options after other treatments failed.
Even more surprising: these drugs help people with heart failure even if they don’t have diabetes. The DAPA-HF and EMPEROR-Preserved trials showed dapagliflozin and empagliflozin cut hospitalizations for heart failure by about 30%, regardless of whether the patient had type 2 diabetes. That’s why cardiologists now prescribe them for heart failure patients across the board.
Common Side Effects: Infections and Dehydration
With benefits come trade-offs. The most common side effects are genital yeast infections and urinary tract infections. About 6 to 11% of women taking these drugs get yeast infections, compared to just 1 to 2% on placebo. Men get them too-less often, but still noticeably more than usual. These aren’t life-threatening, but they’re annoying enough that many people stop taking the drug. Recurrent infections were the top reason one patient on Drugs.com quit Farxiga after six months, even though her blood sugar was under control.
Another issue is volume depletion. Because you’re peeing out more sugar and fluid, you can get dehydrated-especially if you’re older, on diuretics, or skip meals. This can lead to dizziness, low blood pressure, or even acute kidney injury. The FDA requires a black box warning for this risk. Doctors now tell patients to drink more water, avoid excessive alcohol, and hold the medication during illness or surgery.

The Rare but Serious Risk: Euglycemic Diabetic Ketoacidosis
One of the most dangerous, yet underrecognized, risks is euglycemic diabetic ketoacidosis (euDKA). Unlike classic DKA, where blood sugar is sky-high, euDKA happens when blood sugar is only mildly elevated-sometimes even normal. That makes it easy to miss. The body starts breaking down fat for energy, producing toxic ketones. Symptoms include nausea, vomiting, abdominal pain, and confusion.
Studies show euDKA occurs in about 0.1% to 0.3% of SGLT2 inhibitor users, compared to less than 0.1% in those not taking them. Most cases happen during illness, fasting, or after surgery. A 2022 study found 42% of euDKA cases occurred in patients with kidney function above normal. That means even healthy-looking patients aren’t immune. If you’re on one of these drugs and feel unwell, check for ketones with a urine strip or blood test-even if your glucose looks fine.
Who Should Avoid These Drugs
SGLT2 inhibitors aren’t for everyone. They’re not approved for type 1 diabetes-using them there increases ketoacidosis risk dramatically. They’re also not recommended if your kidney function is too low. Most require dose adjustments if your eGFR drops below 60, and should be stopped if it falls below 45. Starting them when eGFR is under 30 is contraindicated.
People with a history of recurrent genital infections or urinary tract infections may want to avoid them unless the benefits clearly outweigh the discomfort. Those with low blood pressure or on strong diuretics should be monitored closely. And while they’re great for weight loss, they’re not a magic solution-patients who combine them with poor diet or inactivity often see diminishing returns.
Cost and Access: A Real Barrier
These drugs are expensive. A 30-day supply costs around $600 out of pocket in the U.S. That’s a major reason why 33% of patients stop taking them within a year. But most insurance plans cover them, and manufacturer assistance programs can bring the monthly cost down to $10-$25. Still, many patients-especially those on high-deductible plans or without insurance-can’t afford them. That’s a problem, because the long-term savings from avoiding heart attacks, kidney failure, and hospital stays far outweigh the drug cost.
Generic versions won’t be available until 2027-2029. Until then, patients need to work with their providers to get prior authorizations or apply for patient support programs. Some clinics now use SGLT2 inhibitors as part of population health programs, prioritizing them for high-risk patients to reduce overall healthcare spending.
How to Use Them Safely
If you’re prescribed an SGLT2 inhibitor, here’s what you need to do:
- Get your kidney function tested (eGFR) before starting and every 3-6 months after.
- Stay hydrated-drink water regularly, especially during hot weather or exercise.
- Watch for signs of infection: itching, burning, redness, or unusual discharge. Treat yeast infections early.
- Know the symptoms of ketoacidosis: nausea, vomiting, stomach pain, confusion, rapid breathing. Test for ketones if you’re sick.
- Hold the medication during acute illness, surgery, or if you can’t eat for more than a day.
- Don’t stop taking it without talking to your doctor-even if you feel fine.
Many patients report life-changing results. One man with heart failure saw his ejection fraction rise from 28% to 42% in 18 months on Jardiance. Another lost 15 pounds and dropped his A1c from 8.2 to 6.8 without changing his diet. But these outcomes aren’t guaranteed. Success depends on using the drug correctly, monitoring for side effects, and staying in touch with your care team.
The Future of SGLT2 Inhibitors
The FDA approved dapagliflozin in October 2023 for chronic kidney disease-even in people without diabetes. That’s a huge milestone. The EMPA-KIDNEY trial showed empagliflozin slowed kidney decline in patients with advanced kidney disease, regardless of diabetes status. Research is now exploring whether these drugs can prevent heart failure in people at high risk but without symptoms yet.
They’re not perfect. They’re expensive. They have side effects. But for the right patient, they’re one of the most powerful tools we have to prevent disability and death from diabetes complications. The question isn’t whether they work-it’s whether you’re getting the right one, at the right time, with the right support.
Can SGLT2 inhibitors cause low blood sugar?
Not on their own. Unlike insulin or sulfonylureas, SGLT2 inhibitors don’t trigger insulin release, so they rarely cause hypoglycemia. But if you take them with other diabetes medications like insulin or glimepiride, your risk increases. Always check with your doctor before combining treatments.
Are SGLT2 inhibitors safe for older adults?
Yes, but with caution. Older adults are more prone to dehydration and kidney changes. Doctors typically start with lower doses and monitor closely. If you’re over 75, have low blood pressure, or take diuretics, your provider may adjust your dose or avoid these drugs altogether.
Do I need to change my diet while taking an SGLT2 inhibitor?
Not strictly, but it helps. These drugs work best when combined with healthy eating and regular activity. You’ll lose more weight and see better heart and kidney protection if you reduce processed carbs and sugar. Don’t think the drug will do all the work-it’s a tool, not a replacement for lifestyle.
Can I take SGLT2 inhibitors if I have kidney disease?
Yes-in fact, they’re now a first-line choice for people with chronic kidney disease and type 2 diabetes. But your dose must be adjusted based on your eGFR. If your kidney function drops below 30, you should stop taking them. Regular monitoring is essential.
What’s the difference between Jardiance, Farxiga, and Invokana?
They all work the same way but have slightly different trial results. Empagliflozin (Jardiance) showed the strongest cardiovascular death reduction. Canagliflozin (Invokana) has a higher risk of amputations and fractures. Dapagliflozin (Farxiga) is approved for heart failure and kidney disease even without diabetes. Your doctor will pick based on your specific risks and medical history.
Why are these drugs so expensive?
They’re still under patent protection-no generics are available until 2027-2029. Manufacturers set high prices because they’re profitable and demand is growing. But most patients pay much less through insurance or patient assistance programs. Ask your pharmacy or provider about savings options.
Next Steps: What to Do If You’re Considering SGLT2 Inhibitors
If you have type 2 diabetes and heart or kidney concerns, talk to your doctor about whether an SGLT2 inhibitor could help. Bring up your history of infections, kidney function, and any recent hospitalizations. Ask for a baseline eGFR test and discuss the pros and cons specific to your situation. Don’t assume they’re right for you-or wrong for you-just because someone else had a good or bad experience.
If you’re already on one, keep your follow-up appointments. Track your weight, fluid intake, and any symptoms of infection or illness. If you feel off, don’t wait-check for ketones and call your provider. These drugs can be life-saving, but only if you use them wisely.
12 Comments
Nigel ntiniDecember 5, 2025 AT 19:03
These drugs are a game-changer for heart and kidney patients-seriously, if you have diabetes and any cardiovascular risk, asking your doc about SGLT2 inhibitors isn’t optional, it’s survival. I’ve seen patients go from barely walking to hiking weekends in 6 months. Just don’t skip the hydration and kidney checks.
Geraldine Trainer-CooperDecember 6, 2025 AT 15:50
So we’re just dumping sugar out the window now? Wild. I mean… I guess if your body’s got too much, why not let it go? Like a detox but with more pee. Still, ketoacidosis sounds like a horror movie plot.
pallavi khushwaniDecember 7, 2025 AT 07:46
I love how medicine is finally treating the whole person, not just the glucose number. It’s not magic, but it’s close. My mom’s on Farxiga and her BP’s down, she’s lost weight, and she’s actually smiling more. No miracle, just good science.
Priya RanjanDecember 7, 2025 AT 16:16
Of course the pharma giants pushed this. They knew the heart and kidney benefits would hook doctors. But let’s not pretend these drugs are safe for everyone. Yeast infections aren’t ‘annoying’-they’re humiliating, and no one talks about how many women quit because of it. Shame on the marketing teams.
Andrew FrazierDecember 8, 2025 AT 10:18
Y’all act like these drugs are some american medical miracle but in reality they’re just repackaged science from the 90s. We got better stuff in the works. Also, why is everyone ignoring the fact that these drugs are basically diuretics with extra steps? Just say it. And yes, I know the trials, but I’ve seen too many patients crash after surgery because they didn’t hold it.
Ashish VaziraniDecember 9, 2025 AT 18:57
These drugs? A Western scam. In India, we’ve been managing diabetes with turmeric, neem, and fasting for centuries-why are we now chasing expensive pills that make you pee sugar? And don’t get me started on the ketoacidosis risk… They don’t even test for ketones in rural clinics. This is profit over people.
Katie O'ConnellDecember 11, 2025 AT 02:58
While the clinical data supporting SGLT2 inhibitors is robust, particularly in the context of cardiovascular mortality reduction and renal protection, the ethical implications surrounding their cost structure and accessibility remain profoundly concerning. The disparity between therapeutic efficacy and socioeconomic feasibility is not merely a logistical challenge-it is a systemic failure of healthcare prioritization.
Nava JothyDecember 12, 2025 AT 14:41
OMG I just started Jardiance and my yeast infection is LITERALLY a nightmare 😭 I thought it was just ‘normal’ but nooo, I had to go to the gyno and now I’m on antifungals and feeling like a science experiment. Also, I lost 4lbs and my BP is better but I’m terrified of ketoacidosis now… I keep checking my pee strips at 3am 😫
Billy SchimmelDecember 12, 2025 AT 19:45
So… you’re telling me the drug that makes you pee out sugar also helps your heart? Huh. Guess that’s why they call it ‘magic’.
Chris ParkDecember 14, 2025 AT 00:14
Let me guess-this article was funded by Big Pharma. SGLT2 inhibitors? A controlled distraction. The real solution is insulin resistance from processed foods and glyphosate in the water supply. You think they want you cured? No. They want you on lifelong meds. Check the FDA’s conflicts of interest. The ketoacidosis cases? They’re being buried. The data’s rigged.
Mansi BansalDecember 14, 2025 AT 21:33
It is imperative to recognize that the commodification of metabolic health has reached an apex wherein pharmaceutical innovation, though scientifically laudable, is increasingly divorced from the socio-economic realities of patient adherence. The exorbitant cost of these agents, juxtaposed against their life-altering benefits, constitutes not merely a market inefficiency, but a moral indictment of contemporary healthcare architecture.
Dan ColeDecember 16, 2025 AT 04:24
People keep saying 'it's not just about blood sugar'-and they're right. But the real revolution isn't the drug. It's the fact that doctors are finally treating diabetes as a systemic disease, not a sugar problem. This is what precision medicine looks like. And yes, it's expensive. But so is dialysis. So is bypass surgery. So is burying someone at 52. We're paying either way.