When your lungs start to feel heavy, your chest aches, and even breathing feels like a chore, you might be dealing with pneumonia. It’s not just a bad cold that won’t go away. Pneumonia is a serious lung infection that fills the tiny air sacs in your lungs with fluid or pus, making it hard to get enough oxygen. Not all pneumonia is the same. The cause changes everything - from how it starts, how it feels, and most importantly, how it’s treated.
Bacterial Pneumonia: The Sudden Onset
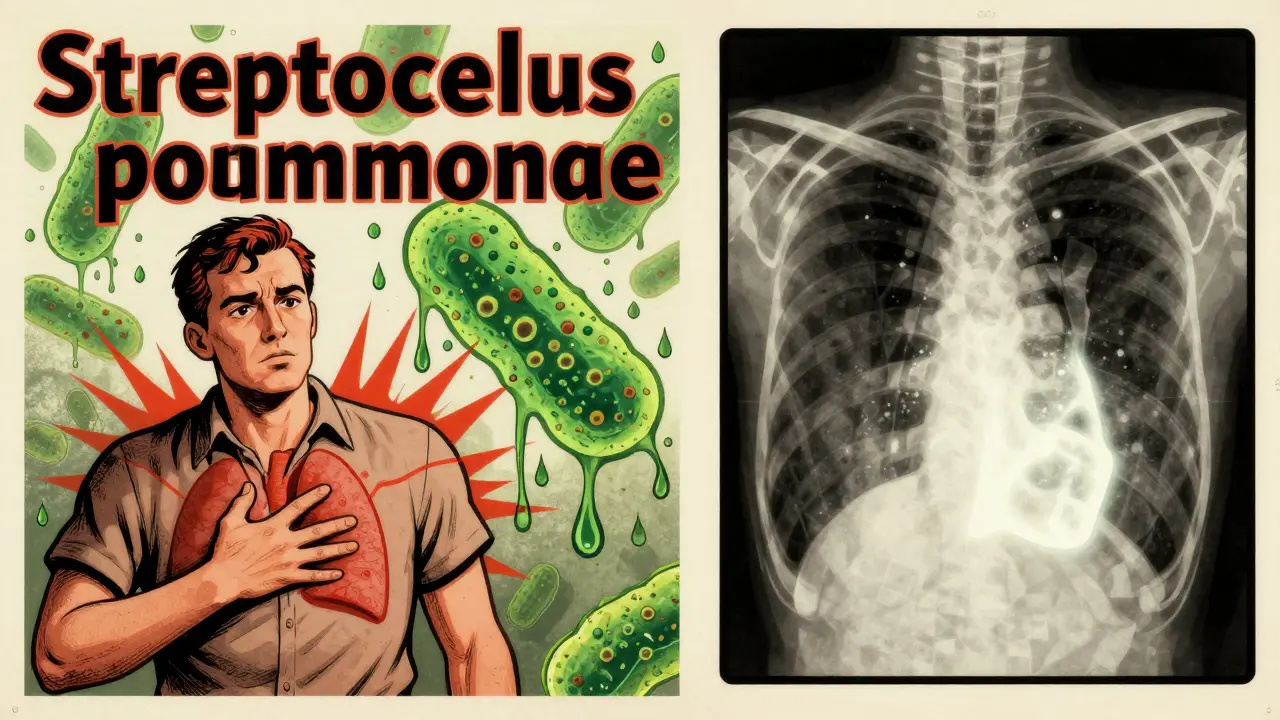
Bacterial pneumonia is the most common type, making up about half of all community cases. The usual suspect? Streptococcus pneumoniae a bacterium responsible for over 12% of severe pneumonia cases in young children and a leading cause across all ages. It doesn’t sneak up - it hits hard. One day you feel fine, the next you’re running a fever of 104°F, shivering, and coughing up thick green or bloody mucus.People often describe the chest pain as sharp, like a knife that gets worse when they breathe in or cough. You might notice your lips or fingertips turning slightly blue - a sign your body isn’t getting enough oxygen. On a chest X-ray, doctors see a solid white patch in one lobe of the lung, called lobar consolidation. That’s the infection, not scattered, but concentrated in one area.
Other bacteria like Staphylococcus aureus, Mycoplasma pneumoniae (the cause of "walking pneumonia"), and Legionella pneumophila (which causes Legionnaires’ disease) can also trigger bacterial pneumonia. Each has its own pattern. Walking pneumonia, for example, doesn’t knock you flat. You might feel tired, have a dry cough, and keep going to work - but you’re still infected.
Treatment is straightforward: antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin are common choices. But here’s the catch - if you take antibiotics when you don’t need them, you’re helping bacteria become stronger. That’s why getting the right diagnosis matters.
Viral Pneumonia: The Slow Burn
Viral pneumonia accounts for about one-third of all cases. It often starts like the flu. You get a sore throat, runny nose, maybe a low-grade fever. Then, over three to five days, things get worse. Your cough turns dry and persistent. You feel achy, weak, and out of breath even walking to the kitchen.Unlike bacterial pneumonia, the fever rarely spikes above 102°F. You’re not coughing up thick mucus - more like clear or white phlegm. On a chest X-ray, instead of one solid white patch, you’ll see a hazy, spread-out pattern across both lungs. That’s because viruses attack the walls of the airways and the tiny air sacs, causing widespread inflammation, not a localized infection.
The usual viruses? Influenza A and B, RSV (especially in kids and older adults), rhinovirus (the common cold virus), and SARS-CoV-2 (the virus behind COVID-19). In fact, during the peak of the pandemic, viral pneumonia was one of the leading reasons people ended up in the hospital.
Antibiotics won’t help here. Treatment is mostly rest, fluids, and fever reducers. For flu-related pneumonia, antivirals like oseltamivir (Tamiflu) can shorten the illness if taken early. For severe COVID-19 pneumonia, remdesivir might be used in hospital settings.
But here’s the dangerous twist: viral pneumonia can open the door for bacterial pneumonia. About 25-30% of people with severe flu develop a secondary bacterial infection - often with Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely when a viral infection doesn’t improve after a week.
Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. It’s not something you catch from a coworker or your kids. You get it from the environment - soil, bird droppings, dust in certain parts of the country. It’s not contagious. But if your immune system is weak, it can take hold.Three main fungi cause most cases in the U.S.: Coccidioides (Valley fever), Histoplasma capsulatum (histoplasmosis), and Blastomyces dermatitidis (blastomycosis). You’re at higher risk if you’re a farmer, construction worker, landscaper, or live in the Midwest or Southwest. Farmers working around bat or bird droppings are 3.5 times more likely to get infected.
Symptoms can look like bacterial or viral pneumonia - fever, cough, fatigue, chills. But sometimes you’ll also have joint pain, skin rashes, or even nausea. It can take weeks to show up after exposure. That’s why it’s often missed. A chest X-ray might show patchy shadows, not the clear lobar pattern of bacterial pneumonia.
Testing is key. You can’t diagnose fungal pneumonia with a regular swab. Doctors need to check sputum, blood, or tissue samples for fungal spores. Treatment isn’t antibiotics - it’s antifungals like fluconazole, itraconazole, or in severe cases, amphotericin B. These drugs can take months to clear the infection, and for people with HIV or who’ve had organ transplants, lifelong treatment may be needed.
Death rates are higher with fungal pneumonia - 10-15% in immunocompromised patients - because it’s often diagnosed late and harder to treat.
How Doctors Tell Them Apart
Figuring out which type of pneumonia you have isn’t always easy. But doctors use clues from your symptoms, your body, and imaging.Here’s what they look for:
- Speed of onset: Bacterial = sudden. Viral = gradual. Fungal = slow, sometimes over weeks.
- Fever: Bacterial = high (102-105°F). Viral = mild to moderate (100-102°F). Fungal = variable, often low-grade.
- Cough: Bacterial = wet, colored mucus. Viral = dry or clear. Fungal = phlegm, sometimes with blood.
- Chest X-ray: Bacterial = one white lobe. Viral = hazy, both lungs. Fungal = patchy, nodules, or cavities.
- Who’s at risk? Bacterial = all ages. Viral = kids, elderly, unvaccinated. Fungal = immunocompromised, outdoor workers.
Now, there’s new tech helping too. Multiplex PCR tests can check a single sputum sample for 20+ viruses and bacteria at once, with over 95% accuracy. That means faster, smarter treatment - and fewer wrong antibiotics.
Prevention: What Actually Works
You can’t avoid every germ, but you can reduce your risk significantly.For bacterial pneumonia: The pneumococcal vaccine (Prevnar 20 or Pneumovax 23) cuts infection risk by 60-70% in kids and 45-75% in adults over 65. Yet, only 68% of seniors get it. That’s a huge gap.
For viral pneumonia: The flu shot reduces pneumonia risk by 40-60% in good match years. The COVID-19 vaccine cuts pneumonia risk by up to 90% in the first few months after vaccination. Getting both shots every year is one of the smartest health moves you can make.
For fungal pneumonia: There’s no vaccine. Your best defense is awareness. If you work with soil, dust, or bird droppings in high-risk areas, wear a mask. Wet the soil before digging. Avoid disturbing old bat guano in attics or caves. If you’re immunocompromised, talk to your doctor about avoiding high-risk environments.

Why Getting It Right Matters
Misdiagnosing pneumonia isn’t just a mistake - it’s dangerous. Giving antibiotics for viral pneumonia doesn’t help. It just makes bacteria stronger. The CDC says 30% of outpatient antibiotic prescriptions are unnecessary. That’s 30% more people helping create drug-resistant superbugs.And the stakes are high. In the U.S., pneumonia sends 1 million people to the hospital each year and kills about 50,000. Bacterial pneumonia kills 5-7% of hospitalized patients. Viral pneumonia kills 3-5%, but spikes to 9% in the elderly. Fungal pneumonia kills 10-15% in vulnerable people.
Knowing the type isn’t just academic - it’s life-saving. It means you get the right treatment fast. It means you don’t waste time on drugs that won’t work. It means your body has the best shot to heal.
And with new tools like host-response biomarkers - tests that look at your body’s immune signals to tell if an infection is bacterial or viral - we’re getting closer to eliminating guesswork entirely. Research funded by the NIH suggests this could cut unnecessary antibiotic use by 40% in the next five years.
Can you have pneumonia without a fever?
Yes, especially in older adults, young children, or people with weakened immune systems. Instead of fever, they might feel confused, dizzy, or unusually tired. A dry cough or shortness of breath may be the only signs. Don’t wait for a fever to seek help.
Is pneumonia contagious?
The germs that cause pneumonia can be contagious, but pneumonia itself isn’t directly spread like a cold. You can catch the virus or bacteria from someone coughing or sneezing, but whether it turns into pneumonia depends on your immune system, age, and health. Someone with a strong immune system might just get a cold. Someone else might develop pneumonia.
How long does pneumonia last?
It varies. Bacterial pneumonia often improves in 1-3 weeks with antibiotics. Viral pneumonia can take 2-4 weeks to clear, even without treatment. Fungal pneumonia may take months, especially in people with weak immune systems. Fatigue and cough can linger for weeks after the infection is gone.
Can you get pneumonia twice?
Yes. Having pneumonia once doesn’t give you immunity. You can get it again from the same or different germs. That’s why vaccines and avoiding risk factors matter - even if you’ve had it before.
When should you go to the hospital for pneumonia?
Go to the hospital if you have trouble breathing, chest pain that doesn’t go away, a fever over 102°F that won’t break, confusion, bluish lips or nails, or if you’re over 65, under 2, or have a chronic illness like diabetes or COPD. These are red flags.
15 Comments
Himanshu SinghDecember 29, 2025 AT 17:59
This is so helpful! I had no idea fungal pneumonia was a thing outside of movies. I work in construction and we dig up dirt all day-gotta start wearing a mask now. Thanks for breaking it down so simply 😊Jasmine YuleDecember 31, 2025 AT 14:06
I can't believe how many people still think antibiotics fix everything. This post should be mandatory reading for every parent, teacher, and doctor who prescribes without testing. 🙏Greg QuinnJanuary 2, 2026 AT 00:31
It's wild how the body's response to infection is basically a language. Bacterial = fire in one room. Viral = smoke spreading through the whole house. Fungal = mold growing slowly in the basement you didn't know existed. We're still learning how to read it.Lisa DoreJanuary 2, 2026 AT 17:53
To anyone reading this and thinking 'I'm fine'-if you've been feeling off for more than a week, please get checked. I waited too long after my flu last year and ended up in the ER. This info saved my life. You're not being dramatic-you're being smart.Sharleen LucianoJanuary 2, 2026 AT 21:33
Honestly, it's embarrassing how little the average person knows about pulmonary pathology. The fact that 30% of antibiotic prescriptions are unnecessary isn't a statistic-it's a cultural failure. If you can't differentiate between a virus and a bacterium, maybe don't self-diagnose on WebMD.Henriette BarrowsJanuary 4, 2026 AT 01:06
I'm 72 and had pneumonia last winter. No fever. Just... exhaustion. Like my bones were made of wet sand. I thought I was just aging. This article made me cry because I wish I'd known this sooner. Thank you for writing this.Teresa Rodriguez leonJanuary 5, 2026 AT 22:00
I'm just here to say I hate when people act like they're the only ones who've ever been sick. Like you discovered pneumonia. Newsflash: everyone gets sick. Stop posting like you're a doctor.David ChaseJanuary 7, 2026 AT 10:59
This is why America is dying. We let foreigners and liberals tell us what medicine is. In my day, you took penicillin for everything and didn't ask questions. Now we need 20 tests and a PhD to treat a cough? 🤬💉🇺🇸Duncan CarelessJanuary 8, 2026 AT 05:17
I'm a paramedic in rural Scotland. We see this all the time-elderly patients come in with just confusion and no fever. This breakdown is spot on. Would love to see this shared in GP waiting rooms.Nicole K.January 8, 2026 AT 09:41
You people are so irresponsible. If you don't get the vaccine, you're putting everyone else at risk. It's not just about you. You're a danger to society. Stop being selfish.Fabian RieweJanuary 10, 2026 AT 04:47
My uncle had fungal pneumonia after working on a farm in Arizona. Took him 8 months to recover. He’s fine now but still takes antifungals. This post nailed it-especially the part about soil and masks. My dad’s gonna wear one next spring.Amy CannonJanuary 10, 2026 AT 05:45
The ontological implications of pathogenic fungal exposure in anthropogenic environments are profoundly concerning. One must consider not only the biomechanical disruption of alveolar integrity but also the sociopolitical neglect of occupational health protections for agricultural laborers, particularly within the arid southwestern United States, where systemic underfunding of public health surveillance has exacerbated endemic transmission vectors.Jim RiceJanuary 12, 2026 AT 04:57
LMAO so now we're supposed to believe that a virus can cause pneumonia but not be contagious? That's like saying a bullet can kill you but the gun isn't real. This is fake science.Alex RonaldJanuary 13, 2026 AT 23:29
I'm a nurse in the ICU. We see pneumonia kill people every week. The one thing I wish patients knew? If you're wheezing and your lips are blue, don't wait for a fever. Just come in. You don't need to be 'sick enough'.Nisha MarwahaJanuary 15, 2026 AT 09:46
The immunological cascade triggered by fungal spore inhalation in immunocompromised hosts involves Th17 polarization and IL-17-mediated neutrophil recruitment, which explains the delayed presentation and diagnostic challenges. This aligns with recent 2023 studies in JID on endemic mycoses.