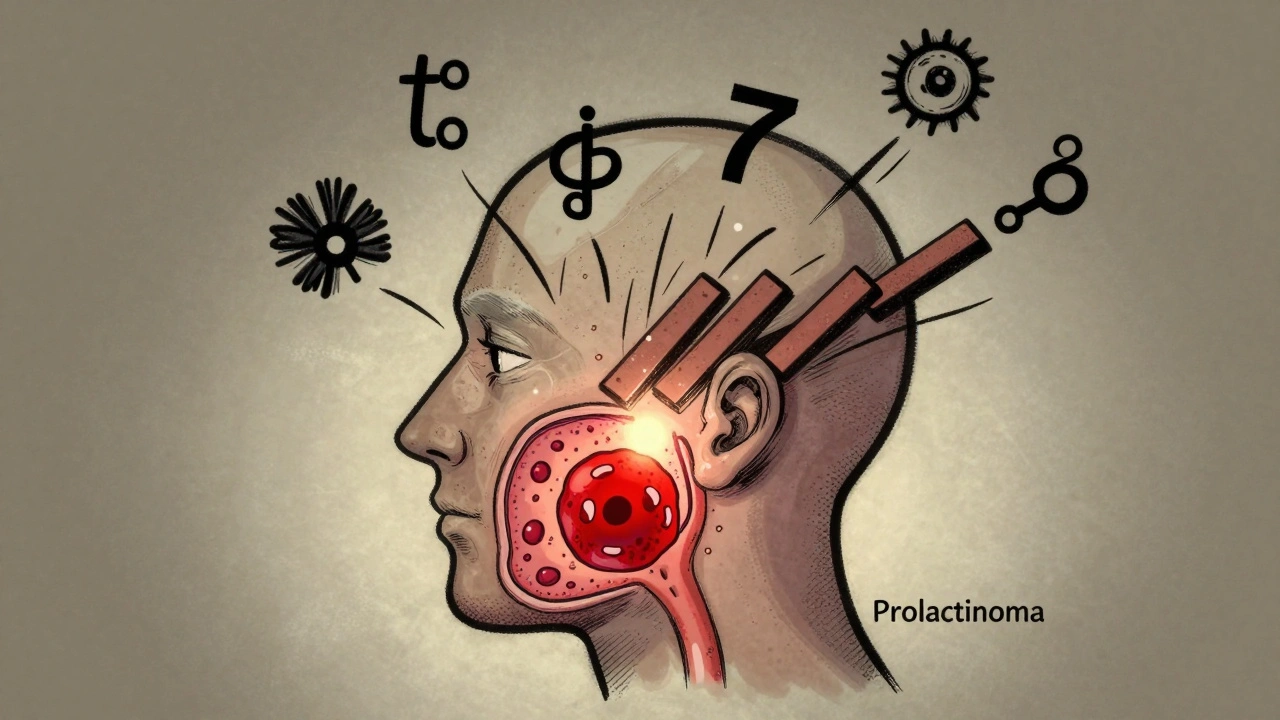
Most people never know they have a pituitary adenoma-until symptoms hit. These small, noncancerous tumors grow on the pituitary gland, a pea-sized organ at the base of the brain that controls nearly every hormone in your body. While many stay quiet and harmless, some, like prolactinomas, start pumping out too much prolactin and throw your whole system off balance. If you’re a woman with unexplained breast milk, missed periods, or trouble getting pregnant-or a man with low libido, erectile issues, or fatigue-you’re not just being ‘stressed.’ You might be dealing with a prolactinoma.
What Exactly Is a Prolactinoma?
A prolactinoma is a type of pituitary adenoma that makes too much prolactin. This hormone normally helps with breast milk production after childbirth. But when it’s overproduced by a tumor, it shuts down other key hormones like estrogen and testosterone. That’s why women often lose their periods, develop breast milk without being pregnant, and struggle with infertility. Men experience low sex drive, erectile dysfunction, and sometimes even breast enlargement. About 40 to 60% of all pituitary tumors are prolactinomas, making them the most common functional type.
Size matters here. Most prolactinomas are microadenomas-under 1 centimeter-and often cause only hormone issues. But if the tumor grows past 1 cm (a macroadenoma), it can press on nearby nerves. That’s when you might lose peripheral vision, get headaches, or even develop double vision. Around 20% of pituitary tumors are this big. And if your prolactin level is over 200 ng/mL, it’s almost always a macroadenoma.
How Do You Know If You Have One?
Diagnosis starts with a simple blood test. If your prolactin level is above 150 ng/mL, the chance it’s a prolactinoma is over 95%. But doctors don’t stop there. High prolactin can also come from stress, kidney failure, or certain medications like antipsychotics or antidepressants. So they rule those out first.
Next comes an MRI of the pituitary gland-with 3mm slices, no exceptions. This shows the exact size and location of the tumor. If it’s larger than 1 cm, you’ll also need a visual field test. This checks if your peripheral vision is being squeezed by the tumor pressing on the optic nerve. It’s quick, painless, and critical.
Don’t ignore symptoms just because they’re embarrassing. A 34-year-old woman in a Mayo Clinic case study had a prolactin level of 5,200 ng/mL-over 100 times normal. She thought her missed periods and milk production were menopause-related. Turns out, it was a 2.4 cm tumor. After six months on cabergoline, her levels dropped to 18 ng/mL. That’s the kind of turnaround you can expect.
First-Line Treatment: Dopamine Agonists
For almost every prolactinoma, the first step is medication-not surgery. Dopamine agonists like cabergoline and bromocriptine trick the tumor into stopping prolactin production. They’re not chemotherapy. They’re targeted, well-studied drugs that have been used for decades.
Cabergoline is the gold standard. It’s taken just twice a week, usually starting at 0.25 mg. Most people see prolactin levels drop within weeks. By three months, 80-90% of microadenomas and 70% of macroadenomas have normal hormone levels. Tumors shrink in 85% of cases. And unlike surgery, it’s reversible if you stop.
Bromocriptine works too, but it’s harder to tolerate. About 30-40% of people get nausea, dizziness, or low blood pressure. That’s why 32% of patients quit it, according to patient forums. Only 18% stop cabergoline. Most people feel better within 4-6 weeks.
Here’s the catch: you usually have to keep taking it. About 70% of patients need lifelong treatment. Stop the pills, and prolactin can bounce back in just 72 hours. That’s why adherence matters. Missing doses isn’t just inconvenient-it’s risky.

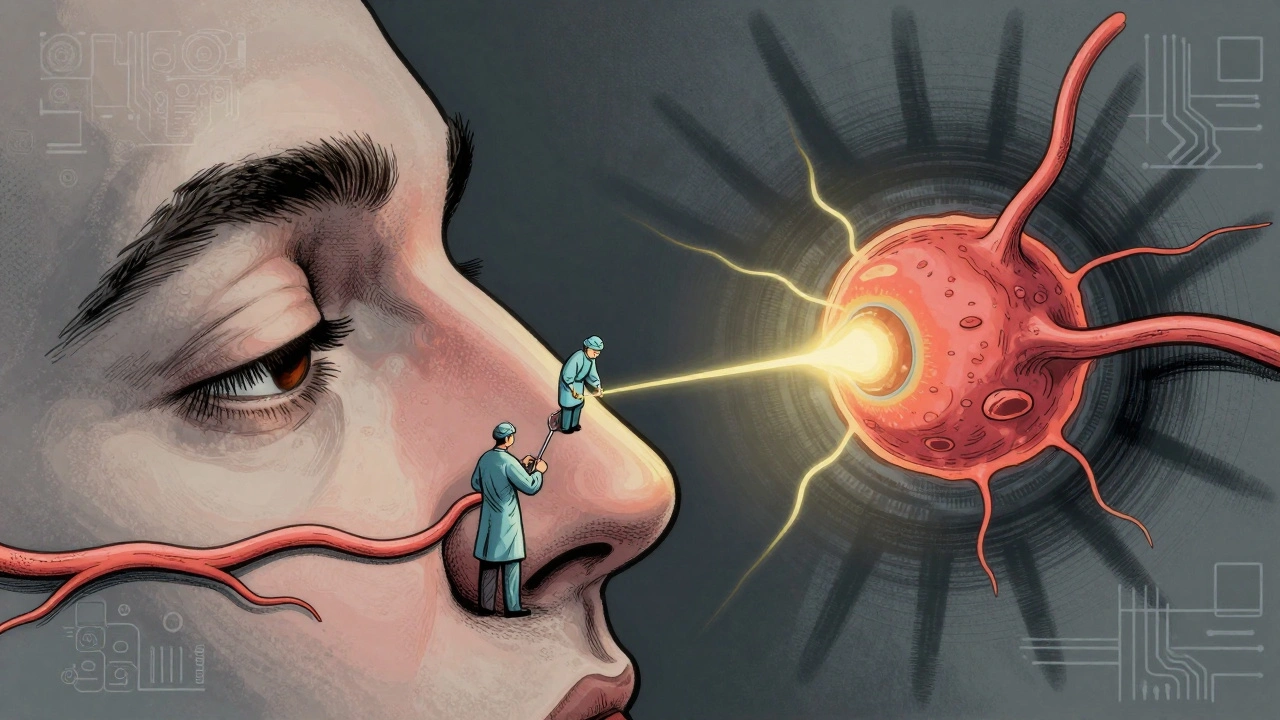
Surgery: When Medication Isn’t Enough
Not everyone responds to pills. Some can’t tolerate them. Others have tumors so big they’re squashing the optic nerve. That’s when surgery comes in.
The standard approach is transsphenoidal surgery-through the nose. Endoscopic tools let surgeons reach the tumor without cutting the face. Recovery is fast: most people go home in 3-5 days. Success rates? Great for small tumors: 85-90% cure for microadenomas. But for macroadenomas? Only 50-60% get fully removed. And even then, recurrence hits 25-30% within five years.
Side effects are real. You might get a cerebrospinal fluid (CSF) leak (2-5% chance), temporary diabetes insipidus (5-10%), or damage to the pituitary gland itself. That means you could need lifelong hormone replacement for cortisol, thyroid, or sex hormones.
Experts agree: surgery should be saved for cases where meds fail, or vision is at risk. Dr. Edward Laws from Brigham and Women’s Hospital says it best: ‘Surgery achieves cure in 85-90% of microadenomas but should be reserved for medication-intolerant patients or those with visual compromise.’
Radiation Therapy: The Slow Option
Radiation is rarely the first choice. It’s slow. It takes 2-5 years to fully work. And it’s not gentle. About 30-50% of patients develop hypopituitarism-meaning their pituitary stops making hormones entirely-within 10 years. That means more pills for life.
But it’s useful for tumors that won’t shrink with meds or surgery. Gamma Knife radiosurgery delivers a precise, high-dose beam in one session. It controls tumor growth in 95% of cases at five years and causes less damage to the optic nerve than traditional radiation.
Patients on forums say they still feel symptoms after a year. But by year three, 85% report improvement. So if you’re considering radiation, you need patience. And you need to accept that you’ll likely need hormone replacement long-term.
What About Long-Term Risks?
Cabergoline is safe for most people-but not at high doses. If you’re taking more than 2.5 mg per day for over three years, your risk of heart valve problems goes up. That’s why the European Society of Endocrinology recommends an echocardiogram every two years if you’re on high-dose cabergoline. The FDA has a black box warning for this, too.
That’s why doctors start low: 0.25 mg twice a week. Then they slowly increase based on your prolactin levels and how you feel. Most people never need more than 1 mg twice weekly.
And yes, you’ll need lifelong monitoring. Even if your prolactin is normal and the tumor shrinks, you’ll get blood tests every 3 months at first, then once a year. You’ll also watch for signs of other hormone problems: fatigue, weight gain, cold intolerance, or dizziness. Those could mean your pituitary is underactive now.
What’s Next? New Treatments on the Horizon
The field is moving fast. In 2023, the FDA approved paltusotine for acromegaly-and early trials show it might work for prolactinomas too. It’s a new kind of pill that targets hormone receptors more precisely.
Researchers are also looking at gene therapies. Some prolactinomas have mutations in genes like MEN1 or USP8. In the next five years, doctors may use genetic testing to pick the best treatment for you-instead of trial and error.
And then there’s AI. Surgeons are starting to use AI to plan tumor removals, predicting exactly where the tumor ends and healthy tissue begins. That could boost success rates for those stubborn macroadenomas.
But here’s the hard truth: 30% of macroadenomas still don’t respond well to current treatments. That’s why research continues. For now, though, most people with prolactinomas do incredibly well-with the right diagnosis and the right pill.
What You Can Do Right Now
If you suspect you have a prolactinoma:
- Get your prolactin level checked. Don’t wait for ‘it’ll pass.’
- If it’s high, ask for an MRI. Make sure it’s done with 3mm slices.
- If you’re a woman with milk and no baby, or a man with low sex drive and fatigue-don’t ignore it.
- Start with cabergoline. It’s effective, easy to take, and well-tolerated.
- Track your symptoms. Note changes in energy, vision, libido, or menstrual cycles.
- See an endocrinologist. This isn’t something a general doctor can manage alone.
Most people with prolactinomas go on to live full, normal lives. The key is catching it early-and sticking with the treatment. It’s not glamorous. But it works.
Can a prolactinoma cause infertility?
Yes. High prolactin blocks the hormones that trigger ovulation in women and sperm production in men. In women, this often shows up as missed periods or inability to conceive. In men, it leads to low sperm count and erectile dysfunction. The good news? Once prolactin levels drop with medication, fertility usually returns. Many patients conceive naturally after starting cabergoline.
Is a prolactinoma cancerous?
No. Prolactinomas are benign tumors. They don’t spread to other parts of the body like cancer. But even though they’re not cancer, they can still cause serious problems by pressing on nerves or disrupting hormone balance. That’s why they need treatment-even if they’re not malignant.
Can I stop taking cabergoline after my prolactin levels normalize?
Some people can, but most can’t. About 30% of patients with microadenomas may be able to stop after 2-3 years if the tumor is gone and prolactin stays normal. But for macroadenomas, the chance of relapse is high-up to 70%. Stopping too soon can cause prolactin to spike again in just 72 hours. Always work with your doctor before making any changes.
Does cabergoline cause weight gain?
Cabergoline doesn’t directly cause weight gain. But if your prolactin was high for a long time, you may have had low thyroid or sex hormone levels, which can slow metabolism. Once treatment starts and hormones rebalance, some people notice weight loss, not gain. Any weight changes are usually tied to improved hormone function, not the drug itself.
How often do I need MRI scans after starting treatment?
After starting cabergoline, your first follow-up MRI is usually after 6-12 months to check tumor shrinkage. If prolactin levels are normal and symptoms are gone, you might only need an MRI every 2-3 years. If the tumor is large or not shrinking, your doctor may scan more often. Always follow your endocrinologist’s plan-don’t skip scans just because you feel fine.
11 Comments
Stacy TolbertDecember 9, 2025 AT 18:23
I had no idea prolactinomas could cause milk production without pregnancy. I thought I was just going through early menopause until my endo ordered the MRI. Turns out my prolactin was 4,800. Cabergoline saved my life. I’m 36 and just got pregnant last month. 🥲
Ryan BradyDecember 11, 2025 AT 14:40
Ugh. Another medical post where the author acts like they’re a doctor. I’ve got a 2.4 cm tumor and I’m still waiting for my insurance to approve cabergoline. Meanwhile, my boss thinks I’m ‘just tired.’ 😒
Raja HerbalDecember 12, 2025 AT 00:46
So let me get this straight - in the US, you need an MRI to prove you’re not just ‘stressed’ about not having sex? In India, we just call it ‘weak nerves’ and give you ashwagandha. 😏
Iris CarmenDecember 12, 2025 AT 15:39
cabergoline is legit. i took it for 8 months and my period came back. also no more milk leaks. weird as hell at first but now i feel like a new person. ty for the post lol
Rich PaulDecember 13, 2025 AT 11:54
Okay but let’s be real - prolactinomas are just pituitary ADHD. Dopamine agonists work because they’re basically brain nerds fixing the feedback loop. Cabergoline = dopamine whisperer. If your tumor’s >1cm, you’re not ‘stressed,’ you’ve got a literal hormone hijack. Also, if your MRI isn’t 3mm slices, you’re getting scammed. Endo’s gotta be neuro-endocrine certified, not just ‘licensed.’
And no, it’s not ‘just a tumor’ - it’s a rogue endocrine node with commitment issues. 70% relapse if you stop meds? That’s not noncompliance, that’s biological betrayal.
And FYI - the FDA black box warning? That’s for people on 5mg/week like they’re taking Adderall. 0.5mg twice a week? Safe as milk. Just don’t skip your echo.
Delaine KiaraDecember 15, 2025 AT 05:23
Okay but imagine being a woman and having to explain to your mom that you’re lactating… but you’re not pregnant. And your husband thinks you’re ‘going through something.’ And then your sister says ‘maybe you’re just stressed’ - and you’ve been crying in the shower for 3 months because you think you’re broken. And then you get the MRI and the doctor says ‘oh, it’s a tumor’ - and you’re like… wait, I have what? A what? In my BRAIN? And then you start the pill and suddenly you’re not a ghost anymore? I’m not even mad. I’m just… relieved. Like, finally, someone named the monster.
And to the guy who said ‘it’s just stress’ - you’re the reason people suffer in silence. I hope you never have to find out what it’s like to feel your body betray you and no one believes you until the numbers prove it.
Ruth WitteDecember 15, 2025 AT 23:30
YOU ARE NOT ALONE 💪💖
My prolactin was 6,200. I thought I was dying. Now I’m 18 months into cabergoline, tumor’s 80% gone, and I just ran my first 5K. 🏃♀️✨
Trust the process. The pill is your new best friend. And yes, you can get pregnant. I did. Twice. 🤰👶
Don’t give up. Your body is fighting for you - and now you’re fighting back. 💜
Noah RainesDecember 17, 2025 AT 21:23
My ex had this. She stopped taking cabergoline after 6 months because she ‘felt fine.’ Three weeks later, her prolactin was back at 4,000. She cried for a week. Then went back on it. Don’t be her. Just take the damn pill. 😑
Katherine RodgersDecember 19, 2025 AT 16:07
Wow. So the real villain here isn’t the tumor - it’s the medical system that makes you wait 8 months for an MRI because ‘it’s not urgent.’ And then when you finally get the diagnosis, you’re told you’re on meds for life? Great. Just great. Meanwhile, Big Pharma is quietly laughing all the way to the bank. 🤡
Gilbert LacasandileDecember 21, 2025 AT 09:22
Thanks for laying this out so clearly. I’ve been reading up on this for my sister - she’s been struggling for years. This is the first time I’ve seen a post that actually explains what’s happening without sounding like a textbook. Really appreciate it.
Lola BchoudiDecember 21, 2025 AT 23:38
As an endocrinology nurse, I’ve seen this too many times. Patients come in with prolactin levels over 2,000, thinking it’s PCOS or depression. The key is early MRI with 3mm slices - anything less and you’re missing microadenomas. Cabergoline is 90% effective. But compliance? That’s the real game. Set phone alarms. Use pill organizers. Tell someone. This isn’t optional - it’s life-changing. And yes, fertility returns. I’ve had 12 patients conceive naturally after starting treatment. You’re not broken. You’re treatable. 💉❤️