Co‑Amoxiclav is a fixed‑dose combination of amoxicillin and clavulanic acid that expands the antibacterial range of amoxicillin by inhibiting beta‑lactamase enzymes. It’s commonly prescribed for respiratory, urinary, and skin infections where the causative bacteria produce beta‑lactamase.
\n\nTL;DR - Quick Takeaways
\n- \n
- Co‑Amoxiclav adds clavulanic acid to amoxicillin, covering beta‑lactamase‑producing bugs. \n
- Azithromycin works on atypical bacteria and needs once‑daily dosing. \n
- Doxycycline is cheap, oral, and useful for tick‑borne diseases. \n
- Cefuroxime offers a broader Gram‑negative spectrum but is more expensive. \n
- Choose based on infection type, bacterial resistance, patient allergies, and dosing convenience. \n
How Co‑Amoxiclav Works
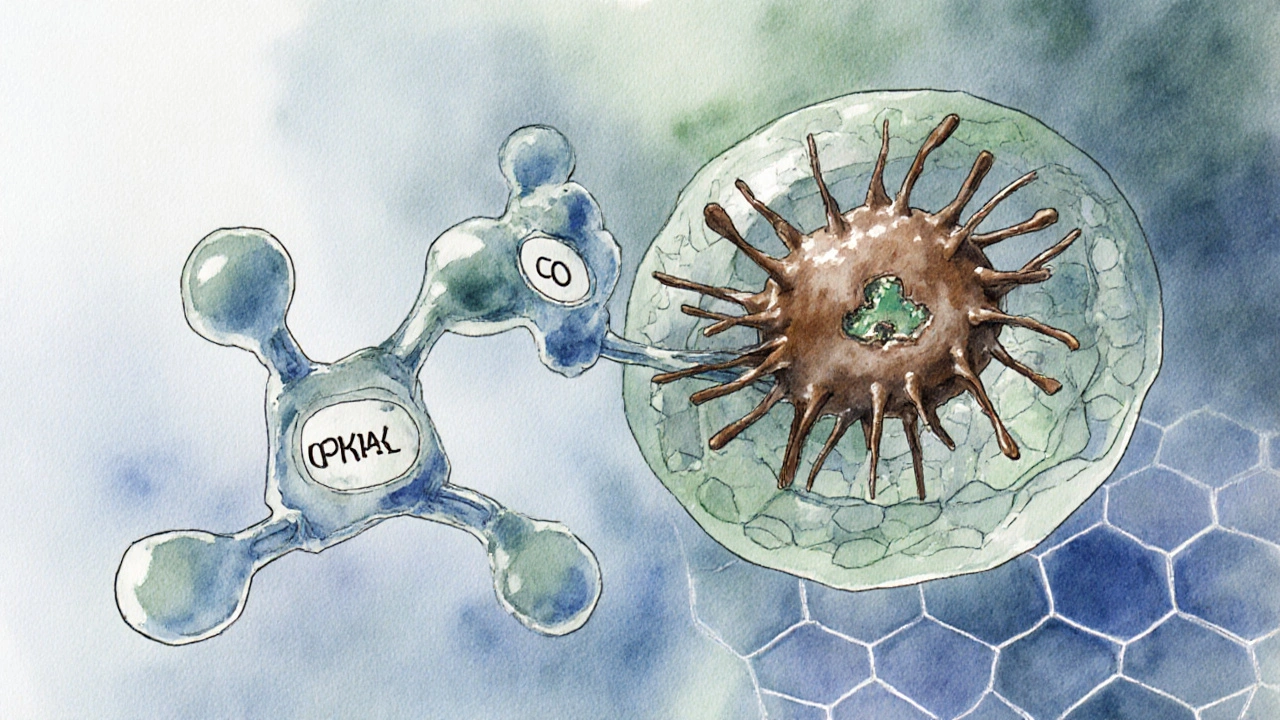
\nThe amoxicillin component interferes with bacterial cell‑wall synthesis, a classic beta‑lactam mechanism. However, many bacteria secrete beta‑lactamase enzymes that break down amoxicillin. The clavulanic acid part is a “suicide inhibitor”: it binds irreversibly to the enzyme, protecting amoxicillin and allowing it to act. This synergy means Co‑Amoxiclav can hit both normal and beta‑lactamase‑producing strains.
\n\nWhen Doctors Prefer Co‑Amoxiclav
\nTypical indications include:
\n- \n
- Acute sinusitis and otitis media where Streptococcus pneumoniae may produce beta‑lactamase. \n
- Community‑acquired urinary tract infections caused by Escherichia coli with known resistance. \n
- Skin and soft‑tissue infections involving Staphylococcus aureus that are not MRSA. \n
It’s not first‑line for simple infections where amoxicillin alone would work, because clavulanic acid adds gastrointestinal side effects and cost.
\n\nKey Criteria for Comparing Antibiotics
\nWhen you line up Co‑Amoxiclav against other options, consider these factors:
\n- \n
- Spectrum of activity - which bacteria are covered? \n
- Resistance profile - is the drug still effective where local resistance is high? \n
- Dosing convenience - number of pills per day. \n
- Safety and side‑effects - especially GI upset, liver impact, or allergic potential. \n
- Cost and availability - generic versions vs brand name. \n
- Special populations - pregnancy, children, renal impairment. \n

Comparison Table: Co‑Amoxiclav vs Common Alternatives
\n| Antibiotic | \nClass | \nTypical Spectrum | \nCommon Indications | \nDosing Frequency | \nFrequent Side Effects | \nApprox. US Cost (30‑day supply) | \n
|---|---|---|---|---|---|---|
| Co‑Amoxiclav | \nBeta‑lactam + beta‑lactamase inhibitor | \nGram‑positive, many Gram‑negative, beta‑lactamase‑producing | \nSinusitis, UTI, skin infections | \nEvery 8h | \nDiarrhea, nausea, liver enzyme rise | \n$12‑$18 | \n
| Azithromycin | \nMacrolide | \nAtypical bacteria, some Gram‑positive | \nChlamydia, atypical pneumonia, traveler's diarrhea | \nOnce daily (5‑day pack) | \nGI upset, QT prolongation | \n$8‑$14 | \n
| Doxycycline | \nTetracycline | \nBroad, covers atypicals, rickettsiae | \nLyme disease, acne, MRSA‑susceptible skin infections | \nTwice daily | \nPhotosensitivity, esophagitis | \n$5‑$10 | \n
| Cefuroxime | \nSecond‑generation cephalosporin | \nGram‑positive, better Gram‑negative than amoxicillin | \nMiddle ear infection, pneumonia, gonorrhea | \nEvery 12h | \nDiarrhea, allergic rash | \n$15‑$25 | \n
| Amoxicillin alone | \nPenicillin | \nGram‑positive, some Gram‑negative (beta‑lactamase‑sensitive) | \nOtitis media, simple sinusitis, dental infections | \nEvery 8h | \nMild GI upset | \n$4‑$7 | \n
When an Alternative Beats Co‑Amoxiclav
\nAzithromycin shines for patients who need a short course and have difficulty adhering to three‑times‑daily dosing. It also covers atypical organisms like Mycoplasma pneumoniae that amoxicillin can’t touch.
\nDoxycycline is the go‑to for tick‑borne diseases (Lyme, RockyMountain spotted fever) and for acne where a long‑term, inexpensive option is required. Its once‑or‑twice‑daily schedule beats Co‑Amoxiclav’s three‑times‑daily regimen.
\nCefuroxime offers a stronger Gram‑negative punch, useful for patients with known beta‑lactamase‑producing Klebsiella or Proteus infections where Co‑Amoxiclav might fall short.
\nIf a patient has a history of liver disease or severe GI intolerance, a simpler beta‑lactam like amoxicillin alone or a non‑beta‑lactam such as azithromycin may be safer.
\n\nSide‑Effect Profile and Safety Tips
\nCo‑Amoxiclav’s most common complaints are diarrhea and nausea, driven by clavulanic acid. About 5% of users report a transient rise in liver enzymes; clinicians usually monitor labs if treatment exceeds two weeks.
\nOther antibiotics bring their own quirks:
\n- \n
- Azithromycin can lengthen the QT interval - avoid in patients on other QT‑prolonging drugs. \n
- Doxycycline causes photosensitivity - advise shade and sunscreen. \n
- Cefuroxime shares the allergy risk of all cephalosporins; cross‑reactivity with penicillin is low but not zero. \n
Always disclose any previous allergic reactions, pregnancy status, or kidney problems before starting therapy.
\n\nChoosing the Right Antibiotic for You
\nThink of the decision as a checklist:
\n- \n
- Identify the likely bacteria (culture results, local resistance patterns). \n
- Check patient‑specific factors - allergy, liver/kidney function, pregnancy. \n
- Match the drug’s spectrum to the bug list. \n
- Weigh dosing convenience against side‑effect tolerance. \n
- Consider cost and insurance coverage. \n
In many primary‑care settings, clinicians start with amoxicillin alone for uncomplicated infections. If symptoms persist or cultures show beta‑lactamase producers, they “step up” to Co‑Amoxiclav. When the infection is known to involve atypical organisms or when a short, once‑daily course is crucial, azithromycin becomes the better pick.
\n\n
Frequently Asked Questions
\nCan I take Co‑Amoxiclav if I’m allergic to penicillin?
\nNo. Co‑Amoxiclav contains amoxicillin, a penicillin derivative. Even a mild penicillin allergy can trigger a serious reaction, so an alternative class should be chosen.
\nHow long should a typical course of Co‑Amoxiclav last?
\nFor most adult infections, 5‑7days is standard. Some deep‑tissue infections may require up to 10days, but extending beyond two weeks increases the risk of liver enzyme elevation.
\nIs Co‑Amoxiclav safe during pregnancy?
\nIt’s classified as Pregnancy Category B (US) - animal studies show no risk, and limited human data haven’t shown harm. Nonetheless, doctors weigh the infection severity against any theoretical risk.
\nWhy does Co‑Amoxiclav cause more stomach upset than amoxicillin alone?
\nClavulanic acid disrupts normal gut flora more aggressively, leading to diarrhea and nausea. Taking the drug with food can reduce irritation.
\nCan I switch from Co‑Amoxiclav to amoxicillin once symptoms improve?
\nSometimes clinicians de‑escalate to amoxicillin if cultures confirm the bacteria aren’t beta‑lactamase producers. This reduces side effects and cost, but the switch should be guided by lab results.
\nBottom line: Co‑Amoxiclav is a solid, broad‑spectrum option when beta‑lactamase‑producing bugs are suspected, but alternatives like azithromycin, doxycycline, or cefuroxime may offer easier dosing, fewer GI issues, or better coverage for specific pathogens. Matching the drug to the infection and the patient’s situation is the key to successful treatment.
17 Comments
Christopher EllisOctober 1, 2025 AT 13:19
Co‑Amoxiclav is just another overhyped combo.
kathy vOctober 4, 2025 AT 11:49
Our nation deserves the strongest weapons against infection and Co‑Amoxiclav is that weapon
It covers a huge range of bacteria and that is exactly what we need to protect our people
But make no mistake, the side‑effects are a price we must pay for safety
We should never settle for half‑measures like amoxicillin alone when the enemy is smarter
And while some argue about cost, the health of our citizens is priceless
Strategic dosing, compliance, and resistance stewardship are all part of winning this battle
Jorge HernandezOctober 7, 2025 AT 10:19
Totally agree with the point about dosing convenience 😊
Three times a day can be a nightmare for busy folks
Switching to a once‑daily regimen like azithromycin really boosts adherence
Just remember to check for QT prolongation as a safety net
Raina PurnamaOctober 10, 2025 AT 08:49
In many cultures, patients value simplicity over broad‑spectrum coverage
Offering a clear explanation of why a short course works helps build trust
Also, be mindful of dietary restrictions that may affect drug absorption
sara vargas martinezOctober 13, 2025 AT 07:19
When it comes to choosing an antibiotic, the decision is rarely as trivial as picking a brand at the pharmacy.
Co‑Amoxiclav offers a broad spectrum that covers many beta‑lactamase‑producing organisms, which is why it often appears at the top of guidelines.
However, the inclusion of clavulanic acid brings a predictable increase in gastrointestinal side effects, a fact that cannot be ignored.
Resistance patterns vary regionally, and in areas with high rates of ESBL‑producing Enterobacteriaceae, even Co‑Amoxiclav may fall short.
Azithromycin, with its once‑daily regimen, provides superior compliance for patients who struggle with thrice‑daily dosing.
Its activity against atypical pathogens makes it indispensible for community‑acquired atypical pneumonia.
Doxycycline, an inexpensive tetracycline, shines in tick‑borne illnesses and offers anti‑inflammatory properties useful in acne treatment.
The drug’s photosensitivity risk, while manageable, requires patient counseling about sun exposure.
Cefuroxime delivers enhanced gram‑negative coverage and is a solid alternative when beta‑lactamase inhibitors are contraindicated.
Cost considerations remain paramount; generic amoxicillin alone can be obtained for a fraction of the price of its combination counterpart.
In patients with a documented penicillin allergy, any beta‑lactam, including Co‑Amoxiclav, poses a significant hazard.
Renal dosing adjustments are essential for agents like cefuroxime to avoid accumulation and toxicity.
Pregnancy categories differ, with amoxicillin generally considered safe, whereas doxycycline is avoided due to potential fetal bone growth inhibition.
Therapeutic de‑escalation from Co‑Amoxiclav to amoxicillin alone is a stewardship practice that reduces adverse events and costs when cultures allow.
Ultimately, the “best” antibiotic is the one that matches the pathogen, patient characteristics, and local resistance data while minimizing harm.
Todd AndersonOctober 16, 2025 AT 05:49
It is incumbent upon the prescriber to weigh the pharmacodynamic merits of the beta‑lactamase inhibitor against the potential for hepatic enzyme elevation.
The inclusion of clavulanic acid confers a broader antimicrobial spectrum, yet the gastrointestinal tolerability profile may be compromised.
Prudent selection, therefore, should reflect both microbial susceptibility and patient-specific factors.
Dexter SmithOctober 19, 2025 AT 04:19
Data suggests that overuse of broad‑spectrum agents fuels resistance trends.
Consider narrowing the regimen once culture data become available.
Emily WagnerOctober 22, 2025 AT 02:49
From a clinical toolkit standpoint, Co‑Amoxiclav is a solid baseline.
But when you factor in adherence hurdles, azithro's once‑daily dosing is a game‑changer.
Don't forget the cost‑benefit matrix for your patient.
Mark FrenchOctober 25, 2025 AT 01:19
Appreciate the concise overview
Just a heads up, some patients report mild stomach upset with the combo
Daylon KnightOctober 27, 2025 AT 22:49
Oh sure, because taking a pill three times a day is exactly what everyone loves to do.
Ellie HartmanOctober 30, 2025 AT 21:19
Great summary for anyone navigating antibiotic choices.
Hope this helps you feel more confident in your decision.
Alyssa GriffithsNovember 2, 2025 AT 19:49
Did you know that the pharma industry, in collusion with regulatory bodies, often skews the data, pushing drugs like Co‑Amoxiclav to the forefront, while suppressing alternatives that could be more effective, safer, and cheaper, especially when you consider the hidden agendas at play?
Cierra NakakuraNovember 5, 2025 AT 18:19
Love how this breaks things down! 👍
Remember to take the meds with food to ease the stomach.
If you ever feel dizzy, let your doc know right away.
Stay healthy!
Sharif AhmedNovember 8, 2025 AT 16:49
Behold, the grand tapestry of antimicrobial strategy, woven with threads of logic and necessity.
Choose wisely, lest the microbes triumph.
Charlie CrabtreeNovember 11, 2025 AT 15:19
👍 Excellent guide!
Hope everyone finds the right fit for their infection! 😊
RaeLyn BootheNovember 14, 2025 AT 13:49
Remember, the cheap option isn’t always the best.
Fatima SamiNovember 17, 2025 AT 12:19
Please note that “Co‑Amoxiclav” should be hyphenated correctly, not “Co‑Amoxaclave”.
Also, “beta‑lactamase” must retain the Greek beta character.