Neuropathic pain doesn’t feel like a cut or a sprain. It’s burning, shooting, or electric - often lasting long after an injury has healed. Around 7 to 10% of people live with this kind of pain, whether from diabetes, shingles, chemotherapy, or nerve damage after surgery. For many, traditional painkillers like ibuprofen or even opioids don’t help. That’s where gabapentin and pregabalin come in. These two drugs are the most commonly prescribed options for nerve pain, but they’re not the same. Knowing the difference can make a big impact on how well your pain is controlled - and how many side effects you deal with.
How Gabapentin and Pregabalin Work
Neither drug is a typical painkiller. They don’t block pain signals like NSAIDs or opioids. Instead, they calm overactive nerves. Both bind to a specific part of nerve cells called the α2δ subunit of voltage-gated calcium channels. When these channels are blocked, fewer pain-signaling chemicals like glutamate and substance P are released. This reduces the "noise" in your nervous system that turns normal sensations into painful ones.
Even though they work similarly, pregabalin binds to this target about six times more tightly than gabapentin. That’s not just a lab detail - it means pregabalin starts working faster and more consistently. Gabapentin was originally developed as an epilepsy drug in the 1990s and later found to help nerve pain. Pregabalin, introduced a decade later, was designed to fix gabapentin’s biggest flaws: unpredictable absorption and slow onset.
Key Differences in How They’re Absorbed
One of the biggest practical differences between these two drugs is how your body handles them.
Gabapentin has what’s called "saturable absorption." That means your body can only absorb so much at once. If you take 300 mg, about 60% gets into your bloodstream. But if you take 1,200 mg, that drops to just 33%. So doubling your dose doesn’t double your pain relief - it might barely help at all. This makes dosing tricky. You can’t just increase the dose and expect better results. Many people end up taking 900 mg three times a day just to get anywhere near a full effect.
Pregabalin doesn’t have this problem. It absorbs nearly 90% of whatever dose you take, no matter how big. Whether you take 75 mg or 600 mg, your body absorbs it reliably. That means your doctor can titrate the dose more predictably. You’ll know what to expect when you increase it - and you’ll usually feel relief faster.
Speed and Consistency of Pain Relief
Time matters when you’re in constant pain.
Gabapentin takes 3 to 4 hours to reach peak levels in your blood. At higher doses, that delay gets even longer. Many patients report waiting 3 to 7 days to feel any benefit - and even then, the effect can be patchy. Some days feel better than others, which is frustrating when you’re trying to plan your life around your pain.
Pregabalin hits peak levels in under an hour. Patients often notice improvement within 24 to 48 hours. In one study, 40% of people with diabetic nerve pain reported at least half their pain gone after just two weeks on pregabalin, compared to only 20% on placebo. That’s not a small difference - it’s life-changing for someone who’s been struggling with burning feet or sharp leg pain for months.
Another advantage? Pregabalin’s pain relief keeps improving as the dose goes up - up to 600 mg per day. Gabapentin hits a ceiling. Once you’re past 1,800 mg a day, adding more doesn’t help much - but it does increase side effects like dizziness and fatigue.
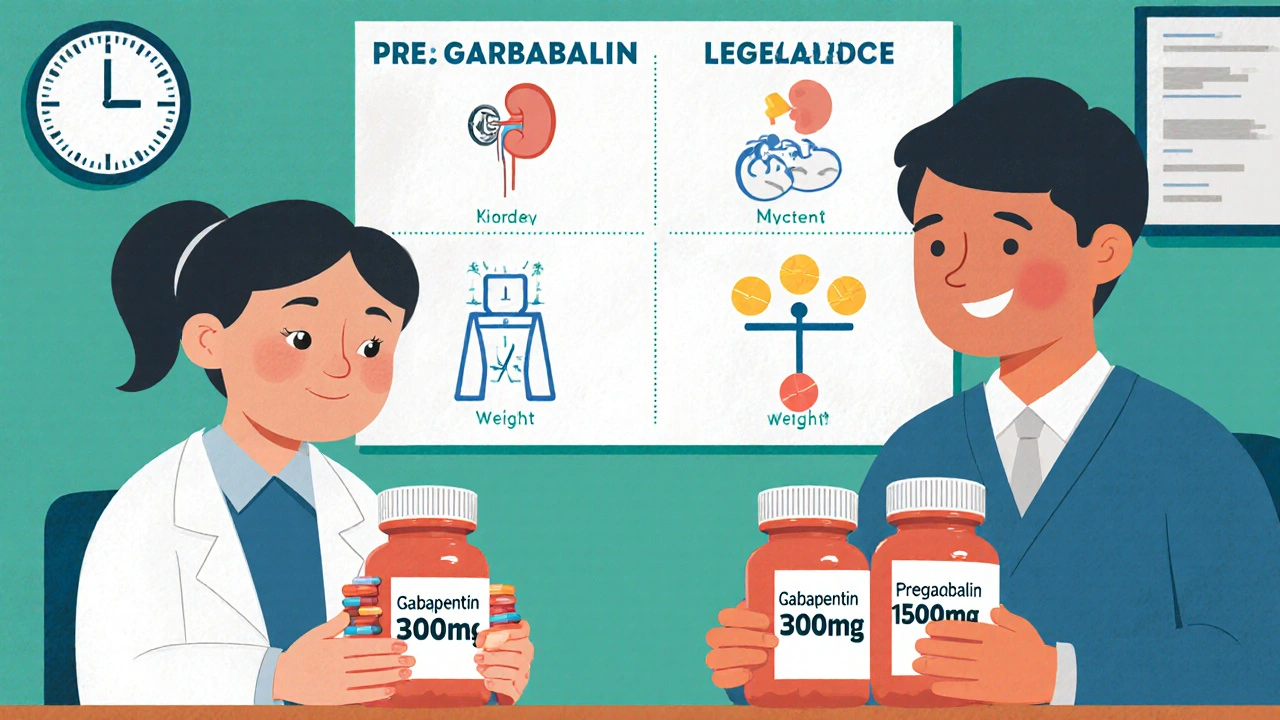
Dosing and Titration: What Your Doctor Will Do
Starting either drug requires patience. You don’t jump to the full dose right away. Too fast, and you’ll feel dizzy, foggy, or unsteady.
For gabapentin, most doctors start at 300 mg once a day, then add another 300 mg every 3 to 7 days. The target is usually between 900 and 3,600 mg daily, split into three doses. That means taking pills three times a day - which can be hard to remember, especially if you’re already managing multiple medications.
Pregabalin starts lower: 75 mg twice a day. After a week, it’s often increased to 150 mg twice a day. Many people stay at 300 mg daily. If needed, the dose can go up to 600 mg daily - still just twice a day. That’s easier to stick with. Some patients even switch from gabapentin to pregabalin just to reduce pill burden.
Renal dosing is another big difference. If your kidneys aren’t working well - common in older adults or people with diabetes - both drugs need lower doses. But with gabapentin, your doctor has to calculate your creatinine clearance and adjust using a complex formula. With pregabalin, there’s a simple table: if your kidney function is below 60 mL/min, you cut the dose in half. That’s much easier for busy clinics to manage.

Side Effects: What to Expect
Both drugs cause similar side effects: dizziness, drowsiness, weight gain, and swelling in the hands or feet. About 30% of people report dizziness with either drug. Weight gain happens in about 25% of users - often around 5 to 10 pounds over a few months.
But there are subtle differences. Pregabalin tends to cause dizziness a bit more often - 32% of negative reviews mention it, compared to 28% for gabapentin. Gabapentin, on the other hand, is more likely to cause mental fogginess or fatigue, especially at higher doses. Some people say gabapentin makes them feel "drugged"; pregabalin feels more like a calm, steady relief.
One surprising point: gabapentin is more likely to cause sleepiness at night. Many patients take it at bedtime because it helps them sleep - and some say it keeps them asleep longer. Pregabalin wears off faster, so some people wake up in the middle of the night with pain returning.
Cost and Accessibility
Cost is often the deciding factor. Gabapentin is available as a generic, and in 2023, a 30-day supply of 300 mg capsules cost less than $10 at most pharmacies. Pregabalin, even as a generic, runs $80 to $150 for the same period. Insurance often requires prior authorization for pregabalin, and some plans won’t cover it unless you’ve tried gabapentin first.
That’s why gabapentin is still prescribed far more often - 68 million U.S. prescriptions in 2022 versus 12 million for pregabalin. But pregabalin brings in more revenue because it’s so much more expensive. For patients on a tight budget, gabapentin is a practical choice. For those with better coverage or who need faster, more reliable relief, pregabalin often pays for itself in better sleep, less missed work, and fewer doctor visits.
Who Benefits Most From Each?
There’s no one-size-fits-all answer. But here’s what works best in real-world practice:
- Choose gabapentin if: You have stable, mild-to-moderate nerve pain; you’re on a tight budget; you need nighttime relief; or you’re in primary care with limited follow-up.
- Choose pregabalin if: You need fast relief (like after surgery or a flare-up); your pain is severe or inconsistent; you’re in a pain clinic; or you’ve tried gabapentin and it didn’t work well enough.
Some patients start with gabapentin and switch to pregabalin if it doesn’t work. Others try pregabalin first if their doctor knows they’ll have trouble sticking to a complex dosing schedule.
New Developments and What’s Coming
The gabapentinoid field isn’t standing still. In 2023, the FDA approved a new extended-release version of pregabalin called Enseedo XR. It’s taken once a day and keeps blood levels steady, reducing the spikes and dips that cause side effects. Early data shows 22% fewer side effects like dizziness compared to regular pregabalin.
Researchers are also working on next-gen drugs that target only the pain-related part of the α2δ subunit - not the parts that cause dizziness or weight gain. Early animal studies show pain relief without the foggy feeling. That could be a game-changer in the next few years.
But for now, gabapentin and pregabalin are still the standard. Both are recommended as first-line treatments by the International Association for the Study of Pain and the European Federation of Neurological Societies. The big question isn’t whether they work - it’s which one works better for you.
When to Talk to Your Doctor
If you’ve been living with nerve pain for more than a few weeks and over-the-counter meds haven’t helped, it’s time to ask about gabapentinoids. Don’t wait until your pain controls your life.
Also, if you’re already on one of these drugs and:
- Your pain isn’t improving after 4 to 6 weeks
- You’re having side effects that bother you
- You’re taking more than 1,800 mg of gabapentin daily and still in pain
- You’re struggling to remember to take pills three times a day
Then talk to your doctor about switching or adjusting. Neither drug is perfect, but the right one can give you back hours - or even days - of your life.
Abuse Risk and Safety Warnings
Both gabapentin and pregabalin carry a risk of misuse, especially when taken with opioids or alcohol. The FDA issued a warning in 2012 and later required a Risk Evaluation and Mitigation Strategy (REMS) for pregabalin in 2020 because of higher abuse potential. Between 2012 and 2021, gabapentinoid-involved overdose deaths tripled. Pregabalin was involved in 68% of those cases, even though it’s prescribed far less often - likely because people who misuse it find it more potent.
If you’re taking these drugs for pain, don’t mix them with alcohol, benzodiazepines, or opioids unless your doctor says it’s safe. Never take more than prescribed. If you feel like you’re becoming dependent, tell your doctor right away.
Can gabapentin and pregabalin be used together?
Doctors rarely prescribe gabapentin and pregabalin together. Since they work the same way, combining them doesn’t usually improve pain control - but it does increase side effects like dizziness, drowsiness, and swelling. If one drug isn’t working well enough, switching to the other is a better strategy than adding both.
How long does it take for pregabalin to start working for nerve pain?
Most people notice some improvement within 24 to 48 hours. Full pain relief usually takes 1 to 2 weeks. Unlike gabapentin, which can take days to build up in your system, pregabalin reaches peak levels quickly, so you’ll feel the difference sooner.
Is pregabalin better than gabapentin for diabetic neuropathy?
Yes, according to major guidelines. Pregabalin has Level A evidence (strongest rating) for diabetic neuropathy based on multiple high-quality studies showing 50% pain reduction in 30-40% of patients. Gabapentin has Level B evidence - probably effective, but with more inconsistent results across trials.
Can I stop taking pregabalin or gabapentin suddenly?
No. Stopping either drug suddenly can cause withdrawal symptoms like anxiety, insomnia, nausea, sweating, or even seizures. Always taper down slowly under your doctor’s guidance, usually over at least one week.
Do these drugs cause weight gain, and can it be prevented?
Yes, weight gain is common - about 25% of users gain 5 to 10 pounds. It’s likely due to increased appetite and fluid retention. Eating a balanced diet, avoiding sugary snacks, and staying active can help. If weight gain becomes a problem, talk to your doctor about switching to another medication like duloxetine or venlafaxine, which don’t cause weight gain.
Are there natural alternatives to gabapentin and pregabalin?
Some people find relief with supplements like alpha-lipoic acid, acetyl-L-carnitine, or capsaicin cream, especially for diabetic neuropathy. But these aren’t as effective as gabapentinoids for moderate to severe pain. They may help as add-ons, not replacements. Always check with your doctor before starting supplements, especially if you’re on other meds.
Final Thoughts
Gabapentin and pregabalin aren’t magic pills. But for millions of people with nerve pain, they’re the difference between suffering and living. Pregabalin is faster, more predictable, and often more effective - but it costs more. Gabapentin is cheaper and still works well for many - if you’re willing to take more pills and wait longer for results.
The best choice isn’t about which drug is "better." It’s about which one fits your life, your pain, and your budget. Talk to your doctor. Ask about dosing, side effects, and alternatives. And don’t settle for pain that won’t go away - there’s help out there.

12 Comments
Erin NemoDecember 2, 2025 AT 14:09
Just took pregabalin for 3 weeks and my burning feet are finally calm. No more midnight wake-ups. Game changer.
Suzanne Mollaneda PadinDecember 3, 2025 AT 18:21
As a neurologist’s assistant, I’ve seen patients switch from gabapentin to pregabalin all the time. The adherence rate jumps when it’s just twice daily. Also, the weight gain is real - but manageable with diet. Don’t let fear stop you from trying.
Bonnie YounDecember 3, 2025 AT 23:47
YOU CAN DO THIS. I was in agony for years. Gabapentin gave me 30% relief but pregabalin? 80%. You’re not broken. You just haven’t found the right tool yet. Keep going. 💪
Alexander WilliamsDecember 5, 2025 AT 01:57
The saturable absorption kinetics of gabapentin are a pharmacokinetic liability, not a feature. The non-linear bioavailability profile renders dose titration statistically unreliable, whereas pregabalin’s linear absorption permits therapeutic precision. This is basic clinical pharmacology.
Kelly EssenpreisDecember 5, 2025 AT 22:37
They’re both just gateway drugs to the pharmaceutical industrial complex. Why not try acupuncture or CBD? They’re hiding the real cure because it’s not patentable
Kenny LeowDecember 6, 2025 AT 06:19
As someone who’s lived with diabetic neuropathy for 12 years, I started on gabapentin. Took 6 months to even feel a flicker. Switched to pregabalin - 3 days later, I slept through the night. Simple as that. Also, the once-daily XR version? Life-changing. 🙌
Lauryn SmithDecember 8, 2025 AT 05:24
I’m so glad this post exists. My mom was on gabapentin for years and thought she was just getting older. Once she switched to pregabalin, she started gardening again. Pain isn’t normal. You deserve relief.
James AllenDecember 8, 2025 AT 21:46
Look, I get it - pregabalin costs more. But if you’re on Medicare or VA, they cover it fine. The real issue? Doctors are lazy. They just prescribe gabapentin because it’s cheap and easy. Meanwhile, you’re suffering. Stop settling.
Amber-Lynn QuinataDecember 10, 2025 AT 09:43
People don’t talk about how these drugs make you feel like a zombie. I gained 20 lbs, lost my motivation, and my husband said I stopped laughing. I’d rather hurt than be numb. This isn’t healing - it’s chemical suppression.
Rachel StantonDecember 12, 2025 AT 04:10
Important note: if you’re on renal dialysis, both drugs require strict dosing adjustments. Pregabalin’s renal table is simpler, but never guess - always get your GFR checked. Also, the new Enseedo XR is a major step forward - less dizziness, smoother effect. Ask your pain specialist.
ariel nicholasDecember 12, 2025 AT 18:29
...and yet... the FDA’s REMS for pregabalin... was implemented... in 2020... after... a 300% surge... in overdose deaths... involving gabapentinoids... which... are... chemically... related... to... GABA... which... is... the... brain’s... primary... inhibitory... neurotransmitter... so... are... we... really... treating... pain... or... just... sedating... the... nervous... system... into... submission...?
Mary NgoDecember 13, 2025 AT 17:13
While I appreciate the clinical breakdown, one must consider the broader geopolitical context: the pharmaceutical monopolies that control gabapentinoid production are largely headquartered in the U.S., yet pricing disparities are weaponized against low-income populations. The fact that pregabalin is 15x more expensive despite near-identical mechanism of action is not a pharmacological issue - it is a moral failure of capitalist healthcare systems. The real question isn’t which drug works better - it’s who benefits from your suffering.