When you hear the word biosimilar, you might think it’s just another name for a generic drug. But that’s not true. Biosimilars aren’t copies like generics-they’re highly similar versions of complex biologic medicines, made from living cells. The FDA doesn’t give them a simple rating like A, B, or C. Instead, they go through a deep, science-heavy process to prove they’re safe and effective. If you’re wondering how the FDA decides which biosimilars can be sold in the U.S., here’s how it actually works.
What Makes a Biosimilar Different From a Generic
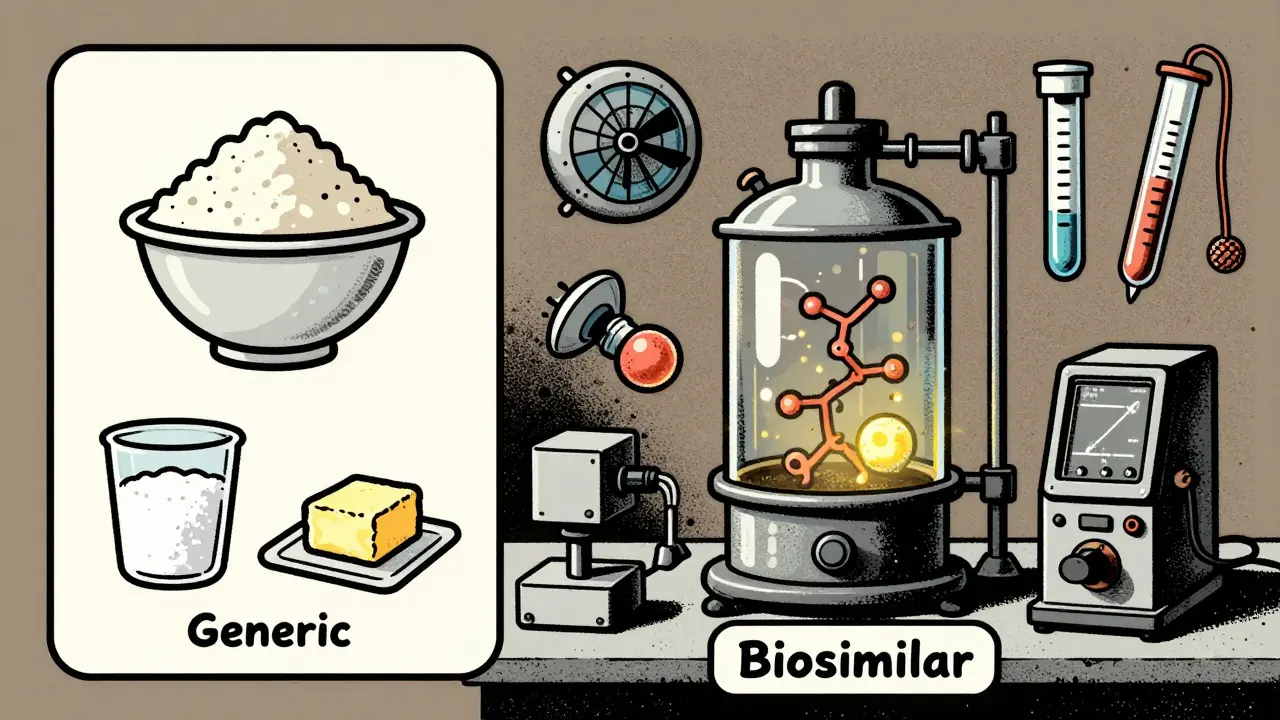
Generics are simple chemical copies of brand-name drugs. You can make them in a lab using the same ingredients every time. Think of them like baking cookies from a recipe-same flour, sugar, butter, same result. Biosimilars are nothing like that. They’re made from living organisms-cells, proteins, antibodies. Even tiny changes in how they’re grown, stored, or handled can change how they work in the body. That’s why a biosimilar isn’t an exact copy. It’s a highly similar version, with no clinically meaningful differences in safety or effectiveness. The FDA requires proof of this similarity through over 200 different analytical tests.The FDA’s Step-by-Step Approval Process
The FDA doesn’t approve biosimilars the same way it approves new drugs. Instead, it uses a special pathway called 351(k), created by the BPCIA in 2010. Here’s how it works:- Analytical studies: Scientists compare the biosimilar to the original biologic using advanced tools like mass spectrometry and capillary electrophoresis. They look at molecular structure, purity, and how the protein folds. The goal? At least 95-99% similarity across critical quality attributes.
- Animal studies: These test for toxicity and how the body reacts. The FDA can skip this step if the analytical data is strong enough.
- Human studies: Pharmacokinetic (how the body processes the drug) and pharmacodynamic (how the drug affects the body) studies are done in 50-100 healthy volunteers. These are usually crossover trials-patients get both the biosimilar and the reference drug at different times.
- Immunogenicity testing: This checks if the body reacts to the drug with unwanted immune responses. This is critical because biologics can trigger antibodies that reduce effectiveness or cause side effects. Testing lasts 24-52 weeks.
The FDA looks at all this data together-the “totality of evidence.” If everything lines up, they approve the product. No large-scale clinical trials with thousands of patients are needed, unlike for brand-new biologics.
The FDA Purple Book: The Official List
You won’t find biosimilars listed in the same place as generics. The FDA’s Purple Book is the only official source for approved biologics and their biosimilars. As of October 2025, it includes 387 reference biologics and 43 approved biosimilars.Each entry shows:
- The reference product name
- The biosimilar’s brand and generic name
- Approval date
- Exclusivity period
- Whether it’s designated as “interchangeable”
Since June 2021, the Purple Book also includes patent information that reference product makers must submit. This helps biosimilar companies plan their launches and avoid legal delays.

Interchangeable vs. Biosimilar: What’s the Difference?
Not all biosimilars are interchangeable. In fact, only 17 out of the 43 approved biosimilars have this status as of late 2025.An interchangeable biosimilar meets an even higher bar. The FDA requires proof that switching between the reference product and the biosimilar won’t increase risk or reduce effectiveness. This means:
- It must produce the same clinical result in any patient
- Switching back and forth multiple times must be safe
- No additional safety risks compared to staying on the reference product
Only interchangeable biosimilars can be automatically substituted by pharmacists without a doctor’s permission-just like generics. The rest require a specific prescription.
Why the FDA’s Process Is Stricter Than Other Countries
The European Medicines Agency (EMA) has approved over 118 biosimilars as of 2025. The FDA has approved only 43. That’s not because the U.S. is behind-it’s because the FDA demands more.According to Dr. Steven Kozlowski, former director of FDA’s Office of Biotechnology Products, the U.S. requires deeper analytical characterization than Europe. That means more tests, more data, and more time. The median approval time in the U.S. is 3.2 years. In Europe, it’s 2.1 years.
But here’s the trade-off: the FDA’s approach has led to zero biosimilar-specific safety signals in over nine years of post-market monitoring. Adverse event rates for biosimilars are statistically identical to their reference products-0.8 per 10,000 patients versus 0.7 for the originals.
Real-World Challenges for Developers
Getting a biosimilar approved isn’t just hard-it’s expensive. The analytical phase alone costs $120-180 million and takes 10-12 months of full-time work by specialized teams. Companies need experts in 10-15 advanced lab techniques.The biggest reason biosimilar applications get delayed? Insufficient analytical data. Especially for complex molecules like monoclonal antibodies, which have intricate sugar structures (glycosylation) that are hard to replicate exactly.
Even after approval, many biosimilars don’t hit the market right away. Patent lawsuits delay launches. Of the 43 approved biosimilars, only 29 have launched as of 2025. The average time from approval to market is 11.3 months.

Market Growth and Where It’s Headed
The U.S. biosimilar market grew from $1.2 billion in 2018 to $12.7 billion in 2024. That’s 18% of the total biologics market. The FDA expects it to hit 30% by 2030, saving patients and insurers $250 billion cumulatively.Oncology biosimilars-like those for rituximab and trastuzumab-are leading adoption. In some cases, they’ve captured 65-75% of the market within 18 months. But in autoimmune diseases like rheumatoid arthritis, uptake is slower. Adalimumab biosimilars, launched in 2023, only reached 28% market share by mid-2025.
Payers and doctors are still cautious. Many prefer to stick with the original brand, even when the biosimilar is cheaper and proven safe.
Recent Changes Making It Easier
The FDA has made major updates to speed things up without lowering standards:- In September 2024, they removed the requirement for comparative efficacy studies in many cases-saving developers $50-100 million per product.
- In June 2025, they allowed indication extrapolation based on analytical data alone, meaning one study can support multiple uses of the drug.
- The Purple Book is now a searchable, API-accessible database with daily updates.
Looking ahead, the FDA plans to release guidance for biosimilars of complex products like antibody-drug conjugates by Q3 2026. They’re also testing AI tools to analyze analytical data faster. By 2027, they aim to have a formal framework for interchangeability of combination products.
What This Means for Patients
You don’t need to understand the science to benefit from it. The bottom line? Biosimilars approved by the FDA are safe. They work just like the original biologics. And they cost 15-30% less.If your doctor prescribes a biosimilar, you’re not getting a lesser drug. You’re getting a scientifically proven alternative that helps lower costs across the system. If your pharmacist switches you to an interchangeable biosimilar, you can trust that it’s been held to the highest standard.
And if you’re prescribed a non-interchangeable biosimilar, you’ll still get the same safety and effectiveness-just with a prescription that specifically names the biosimilar.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs. Biosimilars are highly similar versions of complex biologic drugs made from living cells. They can’t be identical due to their biological nature, but they must have no clinically meaningful differences in safety or effectiveness.
How does the FDA know a biosimilar is safe?
The FDA requires a step-by-step process: detailed lab tests comparing molecular structure, animal studies, human pharmacokinetic trials, and long-term immunogenicity monitoring. All approved biosimilars have been tracked for years-no new safety risks have been found compared to the original biologics.
What does “interchangeable” mean on the FDA Purple Book?
An interchangeable biosimilar has met an extra standard: it can be substituted for the reference product by a pharmacist without the doctor’s permission, and switching between them won’t increase risk or reduce effectiveness. Only 17 of the 43 approved biosimilars have this status.
Why are there so few biosimilars in the U.S. compared to Europe?
The FDA requires more extensive analytical data than the EMA, which makes the approval process longer and more expensive. The U.S. median approval time is 3.2 years versus 2.1 years in Europe. Patent litigation and payer resistance also slow down market entry.
Can I trust a biosimilar if it’s cheaper?
Yes. Lower cost doesn’t mean lower quality. Biosimilars go through a rigorous FDA process that proves they work the same as the original. The savings come from not having to repeat expensive clinical trials, not from cutting corners on safety.
What’s the biggest hurdle for biosimilar developers today?
The biggest challenge is analytical complexity-especially for monoclonal antibodies with intricate sugar chains. Replicating these structures with 95-99% similarity requires advanced lab equipment and years of expertise. Many applications get delayed because the data isn’t detailed enough.
12 Comments
michelle BrownseaJanuary 20, 2026 AT 09:30
Let me be perfectly clear: biosimilars are NOT generics. And anyone who equates them is either dangerously misinformed or willfully ignorant. The FDA’s 200+ analytical tests aren’t a suggestion-they’re a sacred obligation. We’re talking about protein folding, glycosylation patterns, immunogenicity over 52 weeks… this isn’t chemistry class, it’s molecular artistry. If you think cost savings mean cutting corners, you’ve never seen what happens when a monoclonal antibody misfolds in a patient’s bloodstream. No. No. NO.
MARILYN ONEILLJanuary 20, 2026 AT 09:50
So basically the FDA is just being extra? Like, Europe does it faster and nobody dies. Why are we so dramatic? I just want my medicine to work, not read a 500-page lab report before I take it.
Kevin NarvaesJanuary 22, 2026 AT 03:50
fr tho why does it take 3.2 years? like i get the science but its not like we’re launching a rocket to mars. they’re just… copying a drug? why so many tests? i think the fda just likes to feel important. also biosimilars are cheaper so why not just let em in already??
Dee MonroeJanuary 23, 2026 AT 15:50
There’s something profoundly beautiful about how science refuses to cut corners when human lives are on the line. We live in an age where everything is optimized for speed, for profit, for convenience-but the FDA’s insistence on deep, exhaustive, almost obsessive validation of biosimilars? That’s not bureaucracy. That’s reverence. It’s the quiet dignity of a system that says: ‘We will not rush your healing.’ Every analytical test, every week of immunogenicity monitoring, every line of data in the Purple Book-it’s not just regulatory. It’s a moral covenant. And yes, it costs more. And yes, it takes longer. But when your child is on a biologic for juvenile arthritis, you don’t want the fastest path. You want the most certain one. And that’s what this is.
Jerry RodriguesJanuary 23, 2026 AT 23:24
Interesting breakdown. I’ve seen biosimilars used in my clinic and the outcomes are identical to the originals. The real issue isn’t science-it’s trust. Patients and even some doctors still think cheaper means worse. We need better education, not more tests.
Barbara MahoneJanuary 25, 2026 AT 13:02
The Purple Book being searchable and API-accessible is a quiet revolution. For years, this data was locked in PDFs and obscure databases. Now developers, pharmacists, and even patients can trace the lineage of a drug with a few clicks. It’s transparency as medicine.
Amber LaneJanuary 25, 2026 AT 19:02
Interchangeable = pharmacist can swap it. Non-interchangeable = doctor must specify. Simple.
Andrew RinaldiJanuary 26, 2026 AT 15:06
I appreciate how the FDA balances rigor with pragmatism-removing redundant efficacy trials while keeping the core safety checks. That’s smart regulation. Not too much, not too little. Just enough to protect people without stifling innovation.
Samuel MendozaJanuary 28, 2026 AT 02:19
Europe has 118 biosimilars. We have 43. Guess who’s actually helping patients faster?
Yuri HyugaJanuary 28, 2026 AT 05:54
This is why I love science policy 🌟 The FDA isn’t slow-they’re *thorough*. And that’s a gift to patients. Europe moves fast, yes-but the U.S. moves with precision. Think of it like a surgeon: speed saves lives, but accuracy saves *more*. 💪🔬 #BiosimilarsAreNotCheapCopies
Coral BosleyJanuary 28, 2026 AT 18:57
They spent $180 million to prove a drug works like another drug? That’s not science-that’s a corporate extortion racket. The real villains are the big pharma companies holding patents like medieval lords. Let the biosimilars in. People are dying waiting.
Steve HeskethJanuary 29, 2026 AT 14:01
Let me tell you something from Lagos to Los Angeles: when a man in rural Nigeria gets a biosimilar for rheumatoid arthritis at 1/3 the price, he doesn’t care about glycosylation patterns. He cares that he can hold his grandchild again. The FDA’s process is brilliant-but it’s not the whole story. We need global equity, not just perfect science. The real victory isn’t in the Purple Book-it’s in the hands of the person who can finally stand up.