When Your Medications Raise Your Potassium to Dangerous Levels
You’re taking blood pressure pills or heart failure meds because your doctor told you they’ll save your life. But what if those same pills are quietly raising your potassium to dangerous levels-so high that your heart could stop without warning? This isn’t rare. Around 1 in 5 people on common heart and kidney medications develop hyperkalemia, a condition where potassium in the blood climbs above 5.5 mEq/L. At 6.5 mEq/L or higher, it becomes a medical emergency. And many patients don’t feel a thing until it’s too late.
Hyperkalemia doesn’t come with a siren. No burning pain. No fever. Just subtle changes in your heartbeat that most people ignore-maybe a skipped beat, a flutter, or just feeling unusually tired. But behind those quiet symptoms, your heart’s electrical system is being disrupted. Potassium controls how heart cells recharge between beats. Too much, and those cells can’t reset properly. That’s when dangerous rhythms start: irregular pulses, slow conduction, widened QRS complexes on an ECG, and eventually, a sine wave pattern that can flip into ventricular fibrillation-a killer arrhythmia with no warning.
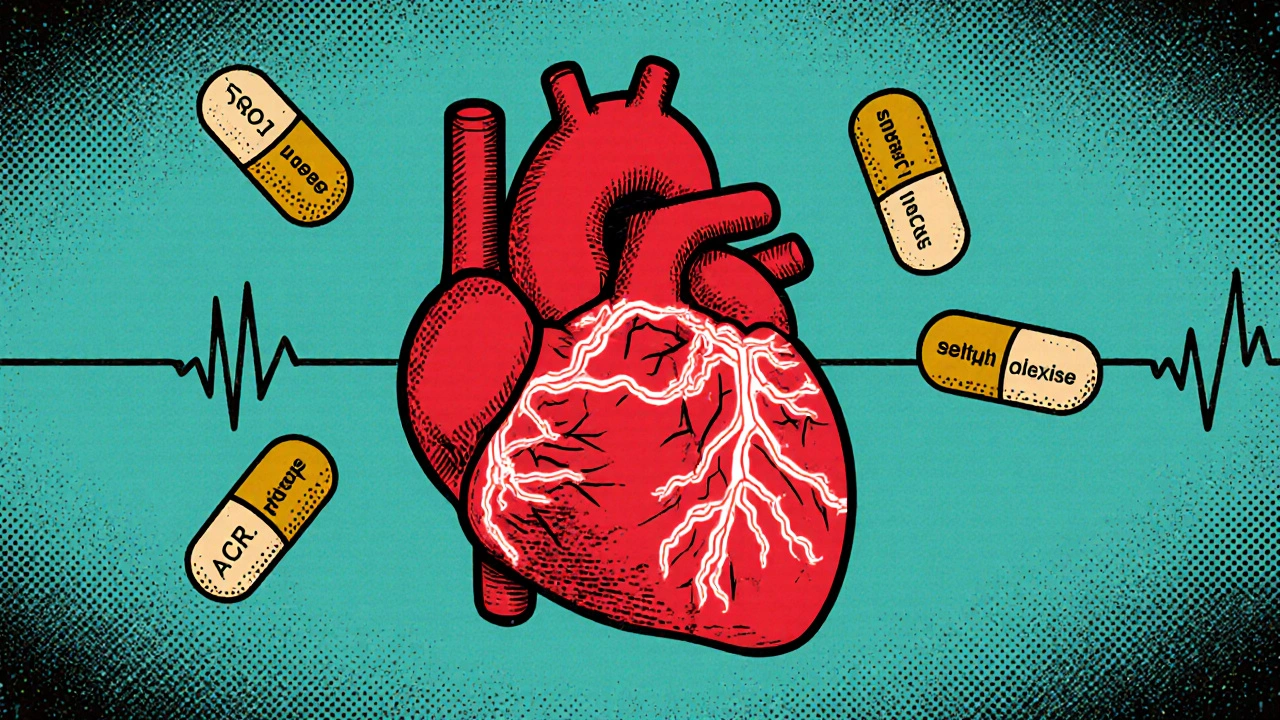
Which Medications Are Most Likely to Cause This?
The real danger isn’t some obscure drug. It’s the very treatments doctors rely on to protect your heart and kidneys:
- ACE inhibitors like lisinopril
- ARBs like losartan
- Mineralocorticoid receptor antagonists like spironolactone
- Potassium-sparing diuretics like amiloride
- Direct renin inhibitors like aliskiren
These drugs work by blocking hormones that raise blood pressure. But they also reduce how much potassium your kidneys flush out. The problem gets worse when you combine them. For example, taking spironolactone with an ACE inhibitor and the antibiotic co-trimoxazole increases your risk of sudden death by over five times compared to spironolactone alone. That’s not a small risk. That’s a red flag.
And it’s not just the meds. Other factors stack the deck: chronic kidney disease (eGFR under 60), diabetes, being over 65, or being dehydrated. Even a mild case of the stomach flu that keeps you from drinking enough water can push potassium levels up in someone already on these drugs.
Why You Might Not Know You’re in Danger
Here’s the scary part: you might not feel anything until your heart starts misfiring. In mild cases-potassium between 5.1 and 6.0 mEq/L-there are often no symptoms at all. People assume they’re fine. But studies show that even mild hyperkalemia leads 38% of patients to stop their heart meds altogether. That’s a huge problem. Stopping ACE inhibitors or ARBs might lower potassium, but it also increases your risk of heart failure hospitalization and death. You’re trading one danger for another.
And it’s not just patients who miss the signs. Some doctors don’t catch it either. ECG changes don’t always show up right away. Peaked T-waves can appear at 5.5 mEq/L, but if the ECG isn’t checked during a routine visit, it’s easy to overlook. PR interval prolongation shows up around 6.5 mEq/L. QRS widening? That’s a red alert above 7.5 mEq/L. By then, you’re in cardiac crisis territory.
What Happens When Potassium Hits 6.5 or Higher?
At 6.5 mEq/L or above, treatment can’t wait. The heart is on the edge. The first step isn’t to lower potassium-it’s to protect the heart right now. That’s where calcium gluconate comes in. Given intravenously over 2-3 minutes, it doesn’t reduce potassium levels. Instead, it stabilizes the heart muscle’s electrical membrane, reversing dangerous ECG changes within minutes. It’s like putting a shield around your heart so it doesn’t go into chaos while you work on fixing the root cause.
After calcium, you need to move potassium from the blood back into cells. That’s done with insulin and glucose: 10 units of regular insulin with 25 grams of glucose IV. This drops potassium by 0.5 to 1.5 mEq/L in 15-30 minutes. Albuterol via nebulizer works similarly, shifting potassium into cells and lowering levels by about 0.5-1.0 mEq/L. These are emergency tools-not cures.
Once the heart is stable, you need to get the excess potassium out of the body. Diuretics like furosemide help if your kidneys are still working. Dialysis is used if kidney function is poor. But here’s the new game-changer: potassium binders.
The New Lifeline: Potassium Binders
For years, the only option when hyperkalemia showed up was to stop the life-saving heart meds. But now, we have drugs that let you keep them.
Patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) are oral binders that trap potassium in the gut and flush it out in stool. They start working within hours. Studies show they lower potassium by 0.4 to 1.0 mEq/L. More importantly, they let patients stay on their RAAS inhibitors. One trial found 86% of patients stayed on their full heart dose with patiromer, compared to just 66% on placebo. That’s a massive win.
These aren’t perfect. About 15-20% of people get constipation. A smaller group gets diarrhea. But compared to the risk of stopping heart meds, they’re a huge improvement. In 2023, the National Kidney Foundation updated its guidelines to recommend these binders as first-line treatment for patients who need to keep their RAAS inhibitors on board.

What You Can Do Right Now
If you’re on any of these medications, here’s what you need to do:
- Ask your doctor for a serum potassium test if you haven’t had one in the last 3 months.
- Know your ECG results. If you’ve had one done, ask if there were any changes-peaked T-waves, widened QRS.
- Don’t take potassium supplements unless prescribed. That includes salt substitutes-many are loaded with potassium chloride.
- Limit high-potassium foods: bananas, oranges, potatoes, tomatoes, spinach, and dried fruit. Aim for 2,000-3,000 mg per day.
- Stay hydrated. Dehydration is a silent trigger.
- If you’re prescribed a potassium binder, take it exactly as directed. It won’t work if you skip doses.
Regular monitoring is non-negotiable. Check potassium levels every 1-4 weeks after starting or changing meds. Once stable, every 3 months is usually enough. But if you get sick, stop eating, or start a new drug-get tested sooner.
The Bigger Picture: Why This Matters
Hyperkalemia isn’t just a lab number. It’s a turning point. For decades, doctors had to choose: protect the heart with ACE inhibitors or protect it from potassium overload. Now, we don’t have to choose. Potassium binders let us do both. And that’s changing outcomes.
Modeling studies suggest that if we reduce RAAS inhibitor discontinuation by even half, we could cut heart failure deaths and hospitalizations by 20-25% in high-risk patients. That’s thousands of lives saved every year in the UK alone.
The goal isn’t to avoid these medications. It’s to use them safely. And that means knowing the signs, asking the right questions, and using the tools we now have to keep your heart protected-not just from high blood pressure, but from the hidden danger inside your own blood.
Frequently Asked Questions
Can hyperkalemia happen without symptoms?
Yes. Many people with mild to moderate hyperkalemia feel nothing at all. That’s why regular blood tests are critical if you’re on medications like ACE inhibitors, ARBs, or spironolactone. Symptoms like fatigue, muscle weakness, or irregular heartbeat often appear only when potassium is already dangerously high.
Is it safe to keep taking my blood pressure pill if I have high potassium?
It depends. Stopping these drugs can increase your risk of heart failure or kidney damage. If your potassium is only mildly high, your doctor may prescribe a potassium binder like Lokelma or Veltassa to keep your levels safe while letting you stay on the medication. These binders are designed specifically to let you keep your heart-protective drugs.
What foods should I avoid to lower potassium?
Avoid or limit bananas, oranges, potatoes, tomatoes, spinach, avocados, dried fruit, nuts, and salt substitutes that contain potassium chloride. Cooking vegetables by boiling them and discarding the water can reduce potassium by up to 50%. A dietitian can help you plan meals that keep potassium under 3,000 mg per day.
How fast do potassium binders work?
Sodium zirconium cyclosilicate (Lokelma) can lower potassium levels within hours-often within 24 hours. Patiromer (Veltassa) takes a bit longer, usually 2-4 days for full effect. Both are taken daily for ongoing control, not just for emergencies.
Can I take over-the-counter supplements if I have high potassium?
No. Avoid all potassium supplements, multivitamins with potassium, and salt substitutes labeled as "lite" or "low sodium"-many contain potassium chloride. Even some herbal teas and energy drinks have added potassium. Always check labels and talk to your doctor before taking anything new.
9 Comments
Lori JohnsonNovember 4, 2025 AT 01:32
I was on lisinopril for years and never knew my potassium was creeping up until I almost passed out at the grocery store. My ECG showed peaked T-waves but my doctor just said "it's fine, keep taking it." Never again. I switched to a binder and now I'm stable. 🙌Tatiana MathisNovember 4, 2025 AT 22:42
This is one of the most important public health messages I've seen in a long time. The fact that patients are being prescribed life-saving medications without routine potassium monitoring is a systemic failure. Many primary care providers don't have the time or training to track this, and patients assume that if they feel fine, everything's okay. But hyperkalemia is silent, insidious, and deadly. The introduction of potassium binders like Lokelma and Veltassa represents a paradigm shift - we no longer have to choose between cardiac protection and electrolyte safety. Regular labs, patient education, and adherence to binders should be standard of care for anyone on RAAS inhibitors. This isn't just clinical knowledge - it's survival literacy.Michelle LyonsNovember 6, 2025 AT 02:17
They don't want you to know this. Big Pharma and the AMA are pushing these drugs because they make billions. Potassium binders? They're expensive. Why not just tell people to stop the meds? But no - they'd rather keep you dependent on $500/month pills and regular blood draws. I've seen the data. The FDA knows. The NIH knows. But they won't tell you. 🕵️♀️Cornelle CamberosNovember 6, 2025 AT 07:49
It is an incontrovertible fact that the widespread prescription of RAAS inhibitors without mandatory potassium surveillance constitutes a gross dereliction of professional duty. The medical literature is unequivocal: hyperkalemia-induced arrhythmia is both preventable and predictable. The failure to implement routine monitoring protocols is not merely negligent - it is criminally irresponsible. One must question the integrity of an industry that prioritizes pharmacological revenue over patient mortality statistics.joe balakNovember 7, 2025 AT 06:15
My potassium was 6.2 last year I was scared but my doctor gave me Lokelma now I'm on all my meds and my numbers are good just take the binder and get testedIván MacedaNovember 7, 2025 AT 23:31
America's healthcare system is broken but at least we have these binders 🇺🇸👏. In other countries they just tell you to stop your meds and die slower. I'm glad we're leading the way. 💪❤️Vrinda BaliNovember 8, 2025 AT 07:35
This is not medicine - this is a slow, silent massacre disguised as treatment. In India, we do not have access to these binders. Our elderly patients are forced to choose between death by heart failure or death by potassium. And still, the Western medical establishment celebrates these drugs as miracles. What is the value of a life if it must be purchased with a $600 pill? The world is watching - and it is ashamed.Rebecca ParkosNovember 8, 2025 AT 16:38
I just got my first potassium binder prescription and I'm so relieved. I was terrified to stop my blood pressure meds but now I don't have to. Thank you for writing this - I shared it with my mom and my sister. We all have diabetes and high blood pressure. This could save our lives. 🤍Bradley MullinerNovember 9, 2025 AT 15:46
People like you who just take binders without questioning why they were put on these drugs in the first place are part of the problem. You're not solving the root cause - you're just buying time with expensive pills. If your kidneys are failing, why are you still on ACE inhibitors? You're not being proactive - you're being obedient. And obedience in medicine is how people die quietly.