Every year, over 2.3 million women worldwide are diagnosed with breast cancer. In the UK alone, about 55,000 new cases are found annually. The good news? More of these cases are caught early - thanks to better screening and clearer guidelines. But with so many recommendations floating around, it’s hard to know what’s right for you. Is mammography still the gold standard? Should you start at 40 or 50? What if your breasts are dense? And once cancer is found, how do doctors decide what treatment to use?
Screening Mammography: The Standard, and the Shift
For decades, mammography has been the backbone of breast cancer screening. It’s not perfect - it can miss some cancers, and sometimes it finds things that turn out to be harmless. But it’s the most proven tool we have to catch breast cancer early, when it’s easiest to treat.
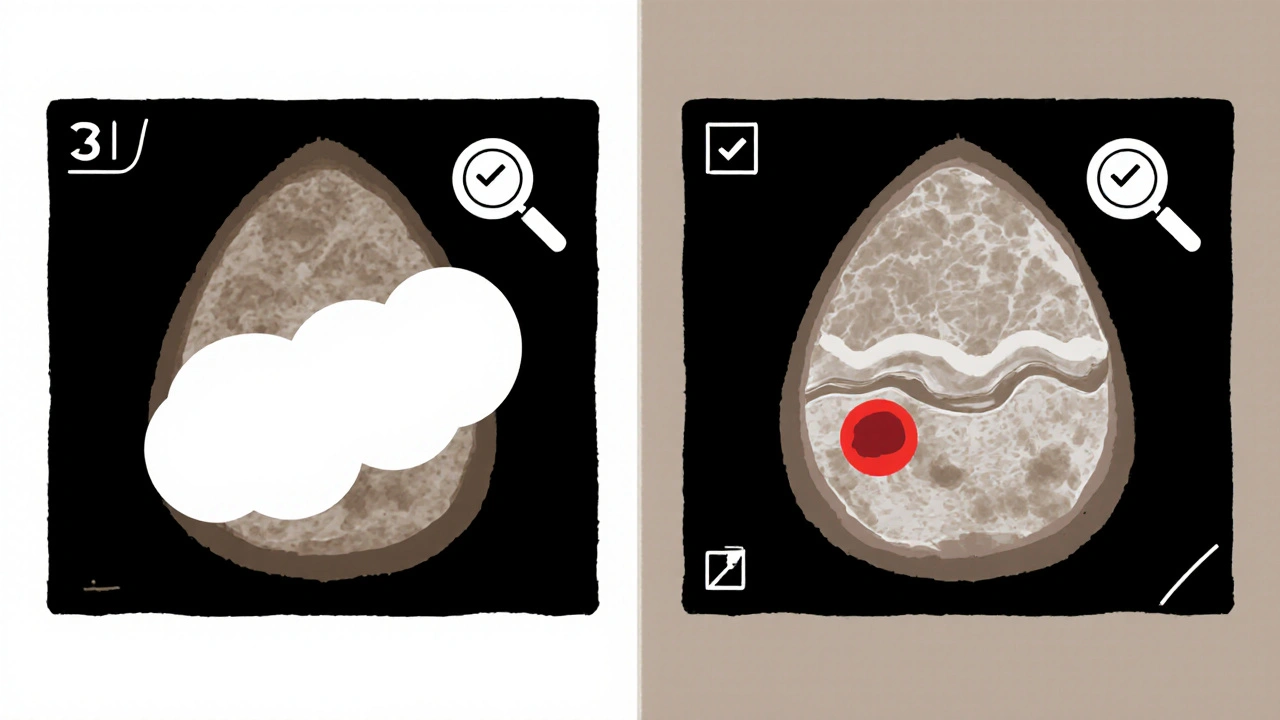
Since the 1960s, mammography has evolved from film to digital, and now to 3D imaging. Digital mammography, or 2D, takes flat X-ray images of the breast. Digital breast tomosynthesis (DBT), or 3D mammography, takes multiple images from different angles and builds a layered 3D picture. This helps doctors see through overlapping tissue, especially in women with dense breasts.
Most women still get 2D mammograms because they’re widely available and covered by insurance. But 3D mammography is becoming the preferred option, especially for those with dense breasts or higher risk. The American Society of Breast Surgeons recommends 3D as the standard for screening. Studies show it finds more invasive cancers and reduces false alarms by up to 40% compared to 2D alone.
Medicare and most private insurers now cover one baseline mammogram and annual screening mammograms. If something looks unusual, diagnostic mammograms - which are more detailed - can be done as often as needed.
When Should You Start Screening? The New Consensus
The biggest change in recent years? The push to start screening at age 40 - not 50.
For years, guidelines were split. The U.S. Preventive Services Task Force (USPSTF) said women aged 50 to 74 should get screened every two years. For those 40 to 49, they said the decision should be personal. But new data changed that.
Since 2020, the number of invasive breast cancers in women under 50 has risen. Studies now show that starting screening at 40 saves more lives than waiting. In fact, a major 2016 meta-analysis found screening reduces breast cancer deaths by about 12% across women aged 39 to 74.
By October 2024, the American College of Obstetricians and Gynecologists (ACOG) updated its guidelines to say: all women at average risk should begin screening at age 40. They recommend mammograms every one to two years, based on shared decisions with your doctor.
This aligns with the American Cancer Society, the National Comprehensive Cancer Network, and the American College of Radiology. Even the American Society of Breast Surgeons says yearly screening should start at 40 and continue until life expectancy drops below 10 years.
That’s the new standard: no more waiting until 50. If you’re 40 or older and haven’t had a mammogram, it’s time to talk to your provider.
What About Dense Breasts? It’s Not Just About Age
One in two women has dense breast tissue - meaning their breasts have more glandular and connective tissue than fat. Dense tissue shows up white on a mammogram, and so do tumors. That makes cancers harder to spot.
The USPSTF says there’s not enough evidence to recommend routine supplemental screening (like ultrasound or MRI) just because your breasts are dense. But other groups disagree.
The American Cancer Society recommends annual mammograms for women with dense breasts, and if they have other risk factors - like a family history or genetic mutation - they should also get an MRI. The American Society of Breast Surgeons says the same: if you have dense breasts, add supplemental imaging.
Here’s what you need to know: if your mammogram report says you have dense breasts, ask your doctor if you should get an ultrasound or MRI in addition to your mammogram. Don’t assume it’s not necessary just because you’re “average risk.”
Who Needs Extra Screening? High-Risk Women
Not all women have the same risk. If you have a strong family history, a known BRCA1 or BRCA2 mutation, had radiation to the chest before age 30, or had certain pre-cancerous breast conditions like lobular carcinoma in situ (LCIS) or atypical hyperplasia, your risk is much higher.
For these women, guidelines are clear: start screening earlier and use more tools.
Most experts recommend:
- Annual mammography starting at age 30
- Annual breast MRI in addition to mammography
- Genetic counseling and testing if you haven’t had it already
The American Cancer Society says women with a lifetime risk of 20% to 25% or higher - calculated using tools like Tyrer-Cuzick or Gail model - should get both MRI and mammogram every year. The American Society of Breast Surgeons recommends formal risk assessment for all women by age 25, and risk modeling should begin at age 30.
If you’ve had breast cancer before, you’ll need ongoing screening - usually every year - and your doctor may recommend different imaging schedules based on your treatment history.
What Happens After a Diagnosis? The Treatment Algorithm
Screening catches cancer early. But once it’s found, what happens next? Treatment isn’t one-size-fits-all. It’s built on a detailed map - called an algorithm - that considers three key things: the cancer’s stage, its biology, and your health.
First, doctors determine the stage using the TNM system: Tumor size, Node involvement, and Metastasis. Is the cancer small and contained? Or has it spread to lymph nodes or other organs?
Then, they test the tumor for three biological markers:
- Hormone receptors (ER/PR): Is the cancer fueled by estrogen or progesterone?
- HER2 status: Is the cancer overproducing the HER2 protein?
- Genomic tests (like Oncotype DX): How likely is the cancer to come back?
These answers guide every decision:
- Early-stage, hormone-positive, low-risk: Surgery (lumpectomy or mastectomy) + hormone therapy (like tamoxifen or aromatase inhibitors). Radiation may be skipped if risk is very low.
- HER2-positive: Surgery + targeted drugs like trastuzumab (Herceptin) + chemo. These drugs have dramatically improved survival.
- Triple-negative: Surgery + chemo. No hormone or HER2 drugs work here. New immunotherapies are now being added for some patients.
For many women, breast-conserving surgery (lumpectomy) is just as effective as mastectomy - especially when followed by radiation. Mastectomy is often chosen for larger tumors, multiple tumors, or genetic risk (like BRCA carriers).
Chemotherapy isn’t automatic. Genomic tests can show whether chemo will add real benefit. For some women, it’s unnecessary. For others, it’s life-saving.

What’s Not Recommended - And Why
Not every test or check helps. Some things you’ve heard about just aren’t backed by science.
Don’t rely on breast self-exams. The Canadian Task Force and USPSTF both say there’s no proof that monthly self-checks reduce deaths. They can cause anxiety and lead to unnecessary biopsies.
Don’t skip mammograms because you’re “too old.” As long as you’re healthy and have a life expectancy of more than 10 years, screening still makes sense. Breast cancer risk increases with age - and older women benefit just as much from early detection.
Don’t use ultrasound or MRI as a replacement for mammography. These are supplemental tools, not stand-ins. Mammography still finds microcalcifications - tiny calcium deposits - that often signal early cancer. Ultrasound and MRI miss those.
What You Can Do Right Now
If you’re 40 or older and haven’t had a mammogram: call your doctor. Ask about 3D mammography if it’s available. If you’re under 40 but have a family history, genetic risk, or dense breasts, ask about risk assessment and earlier screening.
If you’ve been diagnosed: don’t rush. Ask for your tumor’s hormone receptor, HER2, and genomic test results. Ask if you need chemo. Ask if you’re a candidate for breast-conserving surgery. Bring someone with you to appointments. Write down your questions.
Screening saves lives. Treatment works - but only if it’s matched to the right person. The system isn’t perfect, but the guidelines are clearer than ever. You don’t have to guess. You just need to ask the right questions.
Do I still need a mammogram if I have no family history of breast cancer?
Yes. About 85% of breast cancers occur in women with no family history. Screening is based on your age and breast density, not just genetics. Even if no one in your family has had breast cancer, you still have a 1 in 8 lifetime risk. Mammograms are your best tool for early detection.
Is 3D mammography better than 2D? Should I ask for it?
Yes, 3D mammography (DBT) is generally better - especially if you have dense breasts. It reduces false positives by up to 40% and finds 10-20% more invasive cancers than 2D alone. While not every clinic offers it yet, it’s becoming the standard. If your facility has it, ask for it. If not, ask when they plan to upgrade.
I’m 70 and healthy. Should I keep getting mammograms?
If you’re in good health and expect to live more than 10 years, yes. Breast cancer risk keeps rising after 70. Studies show screening still reduces deaths in women up to age 79. The key isn’t age - it’s life expectancy and overall health. Talk to your doctor about whether screening still makes sense for you.
What if my mammogram comes back abnormal?
An abnormal result doesn’t mean you have cancer. Most turn out to be benign. You’ll likely need follow-up imaging - maybe a diagnostic mammogram, ultrasound, or biopsy. Stay calm. Follow your doctor’s plan. Biopsies are quick and safe. Getting answers now is better than waiting.
Can I skip mammograms if I do monthly breast self-exams?
No. Studies show self-exams don’t lower breast cancer death rates. They often lead to false alarms and unnecessary procedures. Mammograms detect tumors too small to feel - sometimes years before they become noticeable. Don’t replace screening with self-checks. Use them as a supplement, not a substitute.
11 Comments
Allison TurnerNovember 27, 2025 AT 22:25
Ugh, another one of those ‘just get a mammogram’ posts. Like that’s gonna fix everything. I’ve had two false positives and one biopsy that turned out to be nothing. My insurance raised my rates after that. Thanks, healthcare system.
Darrel SmithNovember 28, 2025 AT 01:49
Let me tell you something, folks-this isn’t just about medicine, it’s about morality. We’ve let fear and profit drive healthcare into the ground. Mammograms? They’re a billion-dollar industry. And who benefits? Not you. Not me. The corporations. The radiology chains. The pharmaceutical giants. We’re being sold a lie wrapped in a brochure. And now they want us to start at 40? That’s not prevention-it’s panic marketing. My grandmother didn’t have mammograms at 40, and she lived to 92. What’s changed? Nothing but the price tag.
Aishwarya SivarajNovember 28, 2025 AT 13:00
in india we dont even have access to 2d mammograms in most villages and still women die early because they wait till its too late i know a woman who felt a lump but was scared to go to hospital because she thought it was bad luck or punishment i think the real issue is not if we should screen but how do we make it accessible and not scary for women who have never heard of breast cancer before
also 3d is great but if you cant even afford a basic ultrasound whats the point of talking about tomosynthesis
please dont judge women who dont get screened because they dont know or cant afford its not laziness its lack of system
steve stofelano, jr.November 30, 2025 AT 02:23
It is with considerable respect for the evolving clinical consensus that I offer this observation: the integration of 3D mammography as a standard of care represents a significant advancement in early detection methodology. The evidence base, particularly as articulated by the American Society of Breast Surgeons and corroborated by multi-center trials, demonstrates a statistically significant reduction in recall rates and an increase in invasive cancer detection. Furthermore, the alignment of guidelines among major professional societies-including ACOG, ACS, and ACR-indicates a robust convergence of expert opinion. I would respectfully urge all individuals eligible for screening to engage in shared decision-making with their primary care providers, ensuring that individual risk profiles are adequately considered within the framework of evidence-based practice.
Cecily BogsprocketDecember 1, 2025 AT 21:03
I just turned 42 and got my first 3D mammogram last month. I was terrified. Not because I thought I had cancer-but because I didn’t know what to ask. What does ‘dense tissue’ even mean? Should I be worried? Do I need an MRI? I wish someone had told me before I walked in. I’m glad I went. But I also wish this info had been easier to find. You shouldn’t have to google like a detective just to understand your own body.
And if you’re reading this and you’re scared to make that appointment-please just go. You’re not being dramatic. You’re not overreacting. You’re being smart. I cried in the parking lot after. Not because of the results. Because I finally felt like I’d done something right for myself.
Emma louiseDecember 2, 2025 AT 17:00
Oh great, another woke medical guideline. First they told us to wait until 50, now they’re pushing 40 because feminism? Who even decided this? I bet it was some bureaucrat in a lab coat who’s never held a breast in their life. And now they’re saying dense tissue means more tests? That’s just a way to bill more. My cousin got 3 ultrasounds and an MRI and they found nothing. Now she’s traumatized and out $12,000. Wake up, people. This isn’t medicine-it’s profit.
Mira AdamDecember 3, 2025 AT 22:45
Let’s be real: the entire screening industry is built on fear. They tell you to get checked because ‘it saves lives’-but they never tell you how many lives are ruined by false positives, unnecessary surgeries, and anxiety that lasts for years. You think you’re taking control? You’re just feeding the machine. The real enemy isn’t cancer-it’s the illusion that we can control death with machines and algorithms. Maybe instead of scanning every breast, we should be asking why we’re all so afraid to just… live.
Miriam LohrumDecember 4, 2025 AT 03:06
It’s interesting how we treat cancer like an enemy to be defeated, when in reality, it’s just biology gone sideways. We rush to detect, to cut, to zap, to drug-but we rarely pause to ask why our bodies betray us in the first place. Maybe the answer isn’t in more scans, but in how we live. Still… I get why people want the scans. It feels like something you can do. Something that gives you back control. Even if it’s an illusion.
archana dasDecember 4, 2025 AT 20:30
in my village we dont have doctors but we have aunts and neighbors who tell stories and share advice i heard one woman say she felt a lump and her sister told her to massage it with coconut oil and wait it went away after a month i dont know if it was cancer or not but she lived to 80
maybe the real question is not just when to screen but how do we make people feel safe enough to speak up
we need more stories not more machines
Rhiana GrobDecember 6, 2025 AT 01:17
I appreciate the clarity in this post. As someone who works in public health outreach, I’ve seen how confusing guidelines can be-especially when people are bombarded with conflicting messages online. The shift to starting at 40 is a step in the right direction, but we still need better education. Not just about mammograms, but about what dense breasts mean, what the results actually tell us, and how to talk to your doctor without feeling intimidated. Knowledge is power, but only if it’s accessible.
Edward BatchelderDecember 7, 2025 AT 20:48
I'm 73, in great health, and I still get my mammogram every year. I've outlived both of my sisters to cancer. I don't want to be the next one. I'm not doing this for the system. I'm doing it for me. And if you're hesitating because you're scared, or because you think it's unnecessary-just remember: the worst thing that can happen isn't the scan. It's waiting.