Amoeba Infection Risk Calculator
This calculator helps assess your potential risk of amoeba infection based on your activities and symptoms. It's designed to raise awareness and encourage prompt medical attention when needed.
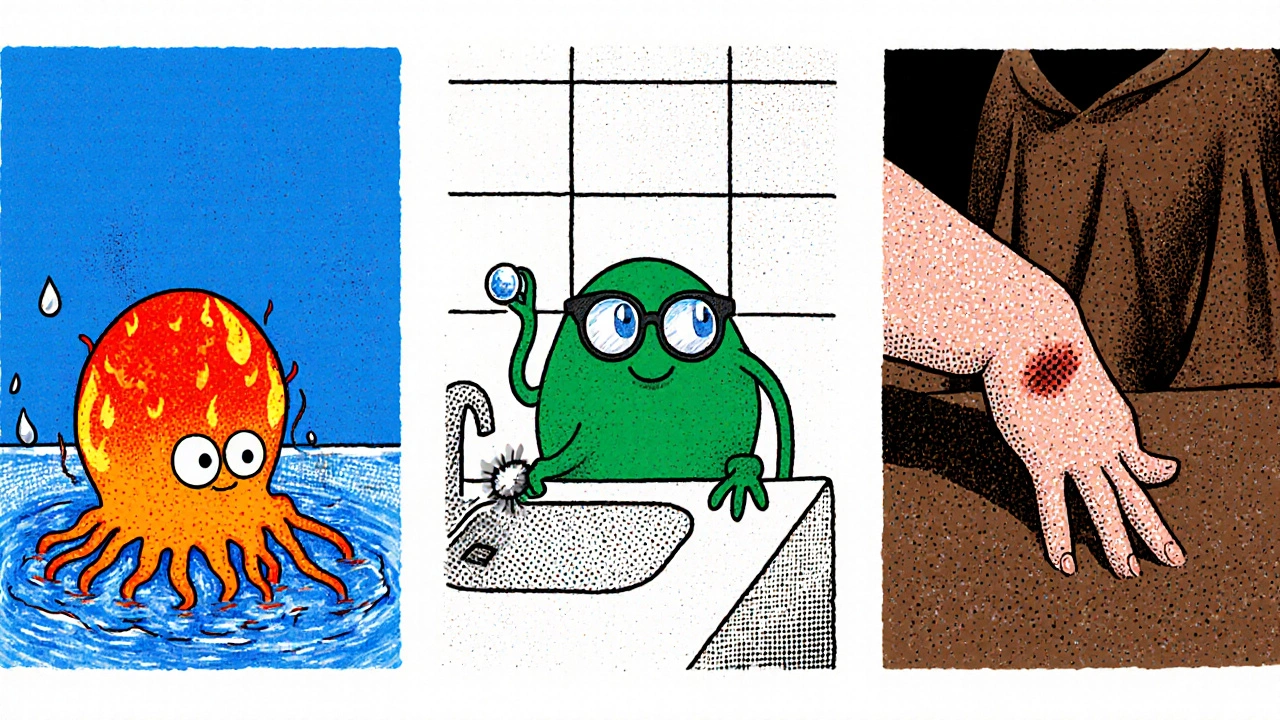
When you hear the word "amoeba," you probably picture a tiny, harmless organism floating in a pond. amoeba infections are, in fact, a growing public‑health concern that claims dozens of lives each year and can affect anyone who swims, uses contact lenses, or works in certain laboratory settings.
What Are Amoeba Infections?
Naegleria fowleri is a free‑living amoeba that thrives in warm freshwater. When it enters the nose during activities like diving or water‑boarding, it can travel up the olfactory nerve to the brain, causing a rapid and often fatal disease called Primary Amebic Meningoencephalitis (PAM).A free‑living, thermophilic amoeba that inhabits warm freshwater bodies worldwide. But Naegleria isn’t the only culprit. Other species such as Acanthamoeba spp. (A group of opportunistic amoebae found in soil, dust, and water that can cause eye, skin, and brain infections.) and Balamuthia mandrillaris (A rare, soil‑borne amoeba that can cause Granulomatous Amebic Encephalitis (GAE).) can also lead to severe disease.
Common Pathogenic Species
Three amoebae account for the overwhelming majority of human cases:
- Naegleria fowleri - causes PAM, an acute meningitis with a mortality rate above 95%.
- Acanthamoeba spp. - associated with Acanthamoeba keratitis (a painful eye infection) and GAE, a slower‑burning brain disease.
- Balamuthia mandrillaris - also leads to GAE, often after skin lesions provide an entry point.
Understanding the biology of each organism helps clinicians spot the right clues early.
How People Get Infected
Exposure routes differ by species. Naegleria fowleri usually enters through the nose during activities that force water up the nasal passages-think swimming in warm lakes, using a neti pot with non‑sterile water, or even high‑pressure dental cleaning. Acanthamoeba finds its way into the eye via contaminated contact‑lens solution, while Balamuthia can breach the skin after a wound contacts contaminated soil or dust.
Because the organisms are everywhere-from municipal water supplies to swimming pools-prevention focuses on simple habits: never submerge your head in warm, stagnant water; always use sterile saline for nasal rinses; and clean contact lenses with recommended solutions.
Symptoms and Clinical Forms
The clinical picture varies dramatically:
- Primary Amebic Meningoencephalitis (PAM): Within 1‑9 days of exposure, patients develop severe headache, fever, nausea, and a rapid decline in consciousness. The disease progresses over hours, often resulting in death within a week.
- Acanthamoeba keratitis: Presents as eye redness, pain, blurred vision, and a characteristic ring-shaped corneal ulcer. If untreated, it can lead to vision loss.
- Granulomatous Amebic Encephalitis (GAE): A slower disease (weeks to months) causing headaches, seizures, and focal neurological deficits. Mortality remains high, but early detection improves outcomes.
Because early symptoms mimic common infections, doctors must keep a high index of suspicion-especially during summer months when water‑related exposure spikes.
Diagnosis
Accurate diagnosis hinges on laboratory techniques that are often unavailable in smaller hospitals:
- Microscopic examination: Direct visualization of trophozoites in cerebrospinal fluid (CSF) is the fastest way to confirm PAM.
- Polymerase chain reaction (PCR): Detects species‑specific DNA in CSF, blood, or tissue samples. PCR has become the gold standard for both PAM and GAE.
- Culture: Growing the amoeba on non‑nutrient agar with a bacterial overlay can identify Acanthamoeba, but results may take weeks.
- Imaging: MRI or CT scans show edema and hemorrhage in PAM, while GAE often reveals multiple ring‑enhancing lesions.
Rapid communication between clinicians and specialized labs (often in major academic centers) saves precious time.
Treatment and Prevention
Therapeutic options remain limited, but recent advances offer hope:
- PAM - The current regimen combines amphotericin B, miltefosine (an antileishmanial drug), and a cocktail of azoles and rifampin. Early administration within 24‑48 hours of symptom onset dramatically improves survival.
- Acanthamoeba keratitis - High‑dose topical chlorhexidine or polyhexamethylene biguanide (PHMB) combined with propamidine is standard. In severe cases, therapeutic keratoplasty may be required.
- GAE - A multi‑drug protocol of pentamidine, azithromycin, fluconazole, and miltefosine has shown success in isolated reports.
Prevention remains the most effective strategy. Public‑health agencies now publish “no‑swim” advisories when lake temperatures exceed 25 °C for prolonged periods. For contact‑lens wearers, the FDA recommends using only sterile solutions and discarding lenses after the prescribed period.
Global Impact and Public Health Response
Although cases are relatively rare-roughly 150 PAM cases worldwide annually-the high fatality rate fuels intense concern. In the United States, the Centers for Disease Control and Prevention (CDC) tracks each case and issues rapid alerts during summer heatwaves. Europe has reported a steady rise in Acanthamoeba keratitis linked to increased contact‑lens use, prompting tighter regulations on solution labeling.
Developing nations face additional challenges: limited laboratory capacity makes diagnosis elusive, and warm climates expand the geographic range of Naegleria. International collaborations, such as the World Health Organization’s Emerging Pathogens Taskforce, are working to standardize case definitions, share diagnostic kits, and train clinicians in low‑resource settings.

Key Takeaways
- Stay out of warm, stagnant freshwater when possible; if you must swim, avoid submerging your head.
- Use sterile water for nasal rinses and follow contact‑lens hygiene guidelines rigorously.
- If you develop severe headache, fever, or eye pain after water exposure, seek medical care immediately and mention the possibility of an amoeba infection.
Awareness, early detection, and prompt treatment are the only weapons we have against these stealthy parasites.
Frequently Asked Questions
Can I get an amoeba infection from a swimming pool?
Yes, if the pool water is warm (above 25 °C) and not properly chlorinated, Naegleria fowleri can survive. Keeping pool chemicals at recommended levels and avoiding submerging your head in hot, stagnant water reduces risk.
What makes Acanthamoeba keratitis different from a regular eye infection?
Acanthamoeba keratitis is caused by a microscopic free‑living amoeba that forms a resistant cyst, making it harder to eradicate. Symptoms include a distinctive ring‑shaped ulcer and intense pain that does not improve with standard antibiotics.
Is there a quick test for PAM?
Microscopic examination of cerebrospinal fluid can reveal motile trophozoites within minutes. However, definitive diagnosis often requires PCR to identify Naegleria fowleri DNA.
How effective is miltefosine in treating these infections?
Miltefosine has become a cornerstone of modern therapy for both PAM and GAE. When started early, survival rates rise from under 5% to roughly 30‑40% in PAM cases, though more data are needed.
What should I do if I suspect I have been exposed?
Seek emergency medical care immediately. Inform the doctor about recent freshwater exposure, nasal rinsing, or contact‑lens use. Early referral to a center with PCR capability can be lifesaving.
Comparison of Major Pathogenic Amoebae
| Feature | Naegleria fowleri | Acanthamoeba spp. | Balamuthia mandrillaris |
|---|---|---|---|
| Typical environment | Warm freshwater (≧25 °C) | Soil, dust, freshwater, tap water | Soil and dust, occasionally water |
| Disease caused | Primary Amebic Meningoencephalitis | Acanthamoeba keratitis, Granulomatous Amebic Encephalitis | Granulomatous Amebic Encephalitis |
| Mortality rate | ~95 % | ~50 % (GAE), low for keratitis with treatment | ~70 % |
| Incubation period | 1-9 days | Weeks to months | Weeks to months |
| First‑line treatment | Amphotericin B + miltefosine + azoles + rifampin | Topical chlorhexidine or PHMB + propamidine | Pentamidine + azithromycin + fluconazole + miltefosine |
Understanding these nuances helps clinicians choose the right diagnostic test and therapy quickly, which can mean the difference between life and death.

12 Comments
Felix ChanOctober 19, 2025 AT 16:36
Hey folks, just a quick reminder to always rinse your neti pot with sterile water – it’s a tiny step that can prevent a nightmare infection. Keep those lenses clean, and you’ll dodge a lot of trouble. Stay safe out there and enjoy the water, just smartly.
Thokchom ImosanaOctober 28, 2025 AT 21:49
The prevailing narrative conveniently omits the clandestine sponsorships that funnel research funds into “ameliorating” amoebic threats while quietly suppressing alternative water‑treatment paradigms. One must consider the geopolitical incentives that drive certain agencies to amplify fear of Naegleria fowleri, thereby justifying exorbitant surveillance budgets. It is not merely a biological hazard but a manufactured crisis engineered by hidden interests. While the public is warned of “warm freshwater dangers,” the same entities manipulate chlorine standards to profit from chemical manufacturers. The veil of scientific objectivity often masks agendas that align with corporate funding streams and nation‑state biowarfare posturing. Hence, critical appraisal of the data sources is essential before accepting the mainstream alarm as unequivocal truth.
Latasha BeckerNovember 7, 2025 AT 04:02
From a clinical microbiology perspective, the trophozoite stage of Naegleria fowleri exhibits rapid thermotolerance, necessitating prompt cerebrospinal fluid sampling for cytological identification. Polymerase chain reaction assays targeting the 18S rRNA gene provide a sensitivity exceeding 95 % and should be instituted alongside conventional microscopy. In contrast, Acanthamoeba spp. form resilient cysts that confer resistance to standard biocides, underscoring the need for polyhexamethylene biguanide regimens in contact‑lens protocols. Balamuthia mandrillaris, albeit rarer, requires tissue biopsy for histopathological confirmation due to its paucity in fluid specimens. Therapeutically, the synergistic administration of amphotericin B, miltefosine, and azole antifungals constitutes the current multimodal approach for primary amebic meningoencephalitis, albeit with variable pharmacokinetic penetration across the blood‑brain barrier. Early interdisciplinary consultation with infectious disease specialists and neurosurgeons markedly improves prognostic outcomes when instituted within the first 24 hours of symptom onset.
parth gajjarNovember 16, 2025 AT 10:16
These parasites are like hidden monsters lurking in every lake they creep into minds of swimmers they drain hope from families their silent assault is terrifying yet we must fight them together
Maridel FreyNovember 25, 2025 AT 16:29
It is crucial for anyone engaging in aquatic activities to adopt evidence‑based preventive measures. First, always avoid submerging the head in warm, stagnant water bodies where thermophilic amoebae thrive. Second, ensure that nasal irrigation devices are filled with sterile or boiled‑then‑cooled water to eliminate potential pathogens. Third, contact‑lens wearers should adhere strictly to manufacturer‑recommended disinfection solutions and replace lenses on schedule. By integrating these practices into routine hygiene, the risk of acquiring a potentially fatal amoebic infection can be substantially reduced.
Madhav DasariDecember 4, 2025 AT 22:42
Totally get the fear, but remember you’re not powerless – a simple pool test kit can flag unsafe temperatures before anyone gets hurt. Share these tips with your crew and keep the vibes positive while staying safe. If you ever doubt the water quality, just skip that dip and plan a cooler adventure elsewhere.
DHARMENDER BHATHAVARDecember 14, 2025 AT 04:56
Prompt diagnosis saves lives.
Kevin SheehanDecember 23, 2025 AT 11:09
The pursuit of knowledge about amoebic pathogens reveals the delicate balance between human curiosity and nature’s indifference. While we devise sophisticated therapies, the organisms persist, reminding us that mastery is provisional. Our ethical responsibility extends beyond treatment to proactive stewardship of environmental resources. If society chooses complacency, the inevitable resurgence will be a stark indictment of collective inaction. Therefore, advocacy for robust public‑health infrastructure is not optional but imperative.
Jameson The OwlJanuary 1, 2026 AT 17:22
There is a concerted effort by global health agencies to downplay the true prevalence of free‑living amoebae. The statistics they release are filtered through political lenses that prioritize economic stability over individual safety. Funding streams are allocated to high‑visibility diseases while leaving amoebic infections in the shadows. Laboratories in remote regions lack the equipment to perform polymerase chain reaction testing, resulting in systematic underreporting. Media outlets receive briefings that emphasize rare cases, creating a false sense of rarity. Meanwhile, private corporations profit from the sale of expensive water‑treatment chemicals marketed as the sole solution. The narrative that only “warm, stagnant water” poses a risk neglects the fact that municipal supplies can harbor cysts despite treatment. Historical documents reveal that similar pathogens were noted centuries ago, yet modern curricula barely mention them. In addition, the CDC’s rapid alert system is throttled during election cycles to avoid public panic. Researchers who publish dissenting data often encounter grant rejections and professional marginalization. The interplay between pharmaceutical interest and public health policy forms a feedback loop that sustains the status quo. Citizens are encouraged to use over‑the‑counter disinfectants rather than demand systemic infrastructure upgrades. When a case does surface, the response is swift but compartmentalized, limiting wider awareness. This selective visibility ensures that the market for antifungal and anti‑amoebic drugs remains lucrative. Moreover, the emphasis on individual responsibility diverts scrutiny from governmental negligence. Consequently, the true burden of amoebic infections remains obscured, perpetuating a cycle of preventable tragedy.
Rakhi KasanaJanuary 10, 2026 AT 23:36
The alarmist tone surrounding amoebic infections often eclipses the nuanced reality that many exposures are mitigated by simple hygiene. While vigilance is commendable, fearmongering can paralyze rather than empower the public. A measured approach that blends education with realistic risk assessment yields better outcomes. Recognizing the role of environmental stewardship alongside personal responsibility is essential. Let us channel our concern into constructive advocacy for improved water safety standards.
Sunil YathakulaJanuary 20, 2026 AT 05:49
Hey folks i get how scary all this sounds but remember you’re not alone in this. Lots of people have already taken steps like using boiled water for nasal rinses and it really helps. If you’re a contact lens wearer make sure you swap out the solution regularly – i’ve seen many cases where lazy cleaning caused big trouble. Also keep an eye on local health advisories before heading out to lakes, they usually post warnings well in advance. Together we can keep the risk low and still enjoy the water responsibly.
Catherine ViolaJanuary 29, 2026 AT 12:02
In light of the foregoing discourse, it is incumbent upon the medical community to adopt a standardized protocol for the early detection of pathogenic amoebae. Uniform implementation of cerebrospinal fluid microscopy, complemented by polymerase chain reaction validation, shall mitigate diagnostic latency. Furthermore, institutional guidelines must delineate mandatory reporting mechanisms to facilitate epidemiological surveillance. It is also advisable that governmental agencies allocate resources toward the development of rapid point‑of‑care assays accessible to peripheral health facilities. By adhering to these rigorously defined measures, we may substantially curtail the morbidity and mortality associated with amoebic encephalitis.