Ivermectin Delivery Method Comparison
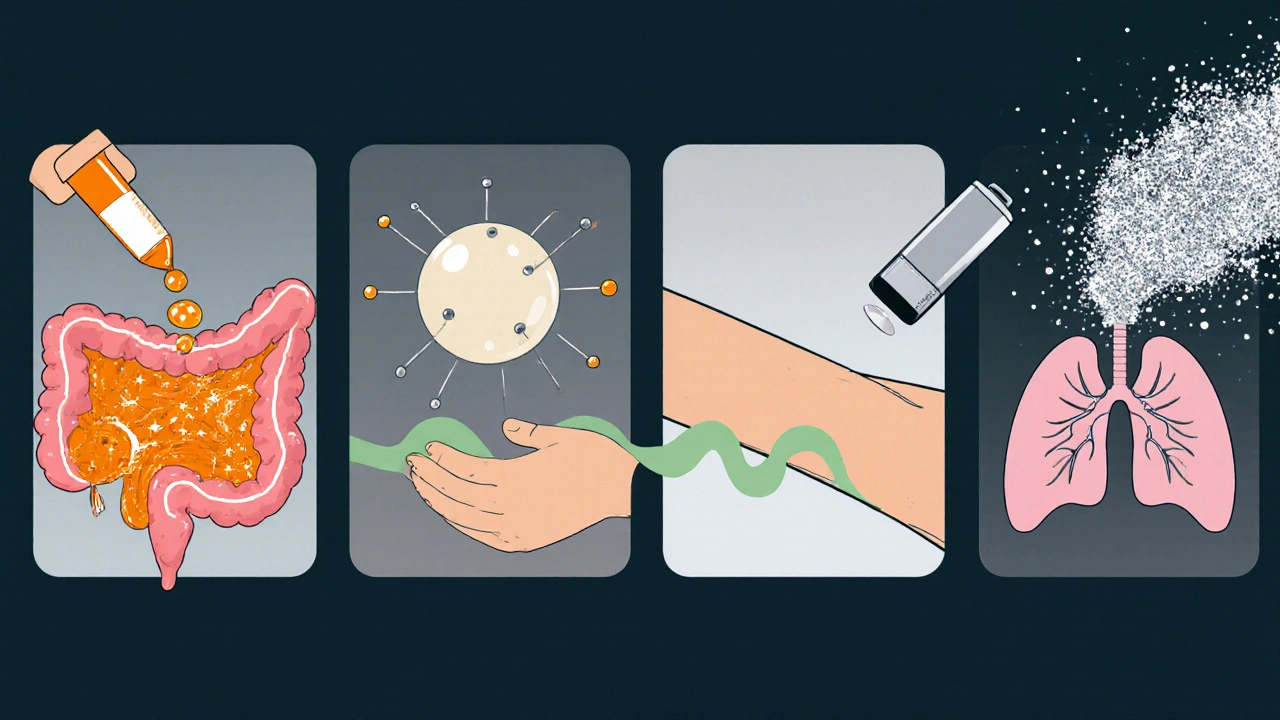
Traditional Oral
Key Feature: Simple tablet administration
Duration: 24-48 hours
Bioavailability: 50-80%
Cost: Low
Adherence: Daily dosing required
Nanoparticle Carriers
Key Feature: Sub-micron carriers (100-200nm)
Duration: Extended release
Bioavailability: Up to 2.3x improvement
Cost: Higher
Adherence: Reduced frequency
Liposomal Encapsulation
Key Feature: Phospholipid vesicles
Duration: Extended release
Bioavailability: Improved
Cost: High
Adherence: Single or infrequent dosing
Transdermal Patches
Key Feature: Skin-adhering patches
Duration: 72+ hours
Bioavailability: 30% increase
Cost: Moderate
Adherence: Single application
Inhalable Powders
Key Feature: Direct lung delivery
Duration: Rapid onset
Bioavailability: 4x higher in lungs
Cost: Moderate
Adherence: Daily or as needed
Implantable Systems
Key Feature: Biodegradable polymer rods
Duration: Weeks to months
Bioavailability: Sustained release
Cost: High
Adherence: Single dose
Key Takeaways
Each delivery method offers distinct advantages and trade-offs:
- Traditional oral remains the most accessible but has significant limitations
- Nanoparticles and liposomes show promise but face scale-up challenges
- Transdermal patches improve adherence but have limited capacity
- Inhalable powders target respiratory infections effectively
- Implantable systems offer the longest duration but require invasive procedures
When scientists look for smarter ways to get Ivermectin where it matters, drug delivery innovations become the star of the show.
Why Revamp Ivermectin Delivery?
Originally approved for treating river blindness and strongyloidiasis, Ivermectin is a broad‑spectrum antiparasitic that also shows activity against certain viruses and bacterial pathogens. Its low cost and wide safety margin make it attractive, but the drug’s pharmacokinetic quirks often limit effectiveness. Traditional oral tablets suffer from erratic absorption, food‑driven variability, and first‑pass metabolism that can drop systemic exposure below therapeutic thresholds.
Researchers therefore turn to delivery science to push more drug into the bloodstream, extend residence time, and target tissues that oral dosing can’t reach. The goal isn’t just higher numbers on a lab report; it’s better outcomes for patients who need reliable, long‑lasting protection.
Traditional Oral Formulation - Limits and Lessons
The classic 150 µg/kg oral tablet is simple, but it reveals three major pain points:
- Variable Bioavailability the fraction of administered drug that reaches systemic circulation ranging from 50 % to 80 % depending on meals and gut health.
- Rapid peak‑and‑fall kinetics that leave drug levels sub‑therapeutic after 24‑48 hours.
- Limited ability to cross the blood‑brain barrier, which hampers treatment of neuro‑parasitic infections.
These shortcomings sparked a wave of formulation research aimed at stabilizing plasma concentrations and boosting overall exposure.
Nanoparticle Carriers: Boosting Bioavailability
Enter Nanoparticle a sub‑micron sized carrier that can encapsulate drugs and protect them from degradation. By shrinking the particle size to 100‑200 nm, researchers increase surface area and improve dissolution in the gastrointestinal tract. A 2023 study from the University of Cambridge showed a 2.3‑fold rise in systemic exposure when ivermectin was loaded into polymeric nanoparticles compared with the standard tablet.
Key advantages include:
- Enhanced solubility in aqueous environments.
- Potential for surface functionalization to target intestinal transporters.
- Reduced dosing frequency thanks to prolonged release.
However, scale‑up challenges and regulatory scrutiny around novel excipients keep nanoparticle formulations in the experimental stage for most markets.
Liposomal Encapsulation: Protecting the Drug
Liposome a spherical vesicle composed of phospholipid bilayers that can carry both hydrophilic and lipophilic substances offers a different protection strategy. Liposomal ivermectin can be administered intravenously or subcutaneously, bypassing the gut entirely. The lipid shell shields the drug from enzymatic breakdown, leading to higher peak plasma concentrations and smoother decline curves.
A Phase II trial in Brazil evaluated a liposomal ivermectin injection for treating strongyloidiasis in immunocompromised patients. The regimen achieved cure rates of 92 % versus 73 % for oral therapy, while adverse events remained comparable.
Drawbacks include higher manufacturing costs and the need for cold‑chain storage, which limits use in low‑resource settings.
Transdermal Patches: Steady Release Through Skin
Skin‑based delivery sidesteps the digestive tract altogether. Transdermal Patch a patch that adheres to the skin and releases drug at a controlled rate can maintain therapeutic levels for days or weeks with a single application.
Recent work from the University of Texas demonstrated a polymer‑matrix patch that released ivermectin at ~0.5 mg per hour for up to 72 hours. Pharmacokinetic modeling showed a 30 % increase in overall exposure and a flatter concentration‑time profile, which is ideal for prophylactic programs in endemic regions.
Advantages:
- Improved patient adherence - no daily pills.
- Reduced peak‑related side effects.
- Potential for combined anti‑inflammatory agents in the same patch.
Skin irritation and limited drug load capacity remain practical concerns, especially for higher dosage regimens.
Inhalable Powders & Nebulizers: Lung‑Targeted Delivery
For respiratory infections where ivermectin’s antiviral properties are under investigation, delivering the drug directly to the lungs can boost local concentrations while keeping systemic exposure modest. Inhalable Powder a dry‑powder formulation designed for aerosolization via a dry‑powder inhaler is one approach; another uses a nebulized solution.
A 2024 pre‑clinical study in ferrets showed that inhaled ivermectin achieved lung tissue levels 4‑times higher than oral dosing, with no detectable toxicity after repeated daily administration for 10 days.
Key benefits are rapid onset and direct targeting of respiratory pathogens. Yet the requirement for inhalation devices and patient technique training can be barriers in community settings.
Implantable and Depot Systems: Long‑Term Control
When a single, long‑acting dose is desirable-such as in mass drug administration campaigns-Implantable Device a biocompatible implant that slowly releases drug over weeks or months becomes attractive. Biodegradable polymer rods loaded with ivermectin have been tested in veterinary medicine, releasing therapeutic amounts for up to 6 months.
Human studies are still early, but the concept promises a “dose‑once, protect‑for‑months” solution that could dramatically cut logistics costs for eradication programs.
Potential risks include surgical insertion, local inflammation, and the need for removal if the implant does not fully degrade.

Choosing the Right Platform: Decision Guide
Not every innovation fits every use‑case. Below is a quick way to match a delivery method to your project goals.
- Rapid systemic exposure needed? - Nanoparticle suspension or liposomal injection.
- Extended prophylaxis with minimal dosing? - Transdermal patch or implantable depot.
- Targeting lung infections? - Inhalable powder or nebulized solution.
- Low‑resource settings? - Keep to oral tablets or simple nanoparticle powders that don’t need cold chain.
Regulatory pathways also differ. The FDA U.S. Food and Drug Administration, the agency that evaluates safety and efficacy of medical products treats nanoparticle and liposome products as new molecular entities, requiring full clinical data, while transdermal patches may follow a 505(b)(2) route if the active ingredient is already approved.
Practical Checklist for Researchers and Developers
Before you start a formulation project, run through this list:
- Define the therapeutic goal: acute cure vs. long‑term prophylaxis.
- Pick a target pharmacokinetic profile (Cmax, half‑life, AUC).
- Assess formulation feasibility: equipment, excipients, scalability.
- Map the regulatory pathway early to avoid surprise data requests.
- Plan stability studies under realistic field conditions.
- Include a patient‑centric usability test - can the intended user apply a patch or inhale a powder correctly?
Following these steps saves months of re‑work and helps align scientific ambition with real‑world impact.
FAQ
Does changing the delivery method affect ivermectin’s safety?
The active molecule stays the same, but how it’s released can influence side‑effects. For example, a rapid IV bolus may cause transient hypotension, while a slow‑release patch usually has milder skin‑related reactions. Each new formulation must undergo its own safety assessment.
Are nanoparticle ivermectin products available commercially?
As of 2025, no nanoparticle‑based ivermectin has received full market approval in major jurisdictions. Several candidates are in Phase I/II clinical trials, especially for veterinary use.
How does a transdermal patch compare cost‑wise to tablets?
Patches are typically 5‑10 times more expensive per dose due to materials and manufacturing complexity. However, when you factor in reduced dosing frequency and lower logistics for mass campaigns, the total program cost can become competitive.
Can inhaled ivermectin treat COVID‑19?
Clinical evidence remains inconclusive. Early in‑vitro studies showed activity, but human trials with inhaled formulations have not yet demonstrated a clear benefit.
What is the timeline for regulatory approval of new ivermectin delivery systems?
A typical pathway, from pre‑clinical work to marketing approval, spans 5‑7 years for novel delivery technologies, assuming no major safety setbacks.
Comparison of Leading Ivermectin Delivery Platforms
| Formulation | Route | Onset (hrs) | Duration (days) | Bioavailability (%) | Typical Dose (mg) | Key Advantage |
|---|---|---|---|---|---|---|
| Standard Tablet | Oral | 1‑2 | 1‑2 | 55‑80 | 200‑400 | Simplicity, low cost |
| Polymeric Nanoparticle Suspension | Oral | 0.5‑1 | 2‑3 | ~150 | 150‑250 | Enhanced absorption |
| Liposomal Injection | IV/Sub‑cut | 0.25 | 3‑5 | ~180 | 100‑200 | Protected from degradation |
| Transdermal Patch | Skin | 2‑4 | 5‑7 | ~130 | 300 (released over time) | Improved adherence |
| Inhalable Powder | Pulmonary | 0.1‑0.5 | 1‑2 | ~120 (lung tissue ↑) | 50‑100 | Targeted lung delivery |
| Implantable Depot | Sub‑cut | 1‑2 | 30‑180 | ~140 | 500‑1000 | Months of protection |

9 Comments
Benedict PosadasOctober 22, 2025 AT 20:13
Yo, this nanotech stuff could finally fix the absorption probs for ivermectin :) Let’s keep pushing these ideas forward!
Jai ReedOctober 24, 2025 AT 13:53
While enthusiasm is appreciated, the regulatory hurdles for nanoparticle excipients are non‑trivial. Companies must submit extensive safety data, and failure to meet standards can delay market entry significantly.
Tim BlümelOctober 26, 2025 AT 06:33
Thinking about drug delivery reminds us that the body is a complex ecosystem; every barrier we cross is a lesson in biology and engineering 🌱. The shift from oral tablets to transdermal patches reflects a broader trend toward patient‑centric solutions. By embracing skin‑based dosing we can improve adherence, especially in remote areas where daily pills are a burden. However, formulation scientists must balance drug load with skin safety to avoid irritation. The future will likely blend multiple platforms for a truly personalized therapy.
Michael VandiverOctober 28, 2025 AT 00:13
Totally agree with you! The patch idea is super cool 😎 and could really change how we think about mass drug admin.
Rachael TurnerOctober 29, 2025 AT 17:53
The ethics of deploying long‑acting ivermectin implants in low‑resource settings merit deep reflection. It's crucial that communities are fully informed and consent to such interventions. Moreover, cost‑effectiveness must be weighed against the need for regular monitoring of potential side effects. A transparent dialogue can bridge the trust gap between researchers and patients.
Suryadevan VasuOctober 31, 2025 AT 11:33
Data from veterinary studies suggest a six‑month release window is feasible, but human trials are still lacking.
Don Goodman-WilsonNovember 2, 2025 AT 05:13
Great, another fancy drug delivery method that only the wealthy can afford-just what we needed.
Diane ThurmanNovember 3, 2025 AT 22:53
Honestly this is just hype, the real issue is that many countries cant even get the basic tablets.
Iris JoyNovember 5, 2025 AT 16:33
The recent wave of ivermectin delivery research showcases how formulation science can overcome long‑standing pharmacokinetic challenges. Nanoparticle carriers, by shrinking the drug into 100–200 nm particles, dramatically increase surface area, leading to faster dissolution in the gut. The Cambridge study you cited demonstrated a 2.3‑fold rise in systemic exposure, which is a compelling proof of concept. However, scaling these polymeric systems from the bench to commercial production remains a bottleneck that many biotech firms are still grappling with. Liposomal encapsulation offers a different route by shielding ivermectin from enzymatic degradation and allowing intravenous or subcutaneous administration. The Phase II trial in Brazil showed impressive cure rates of 92 % compared with 73 % for oral therapy, highlighting the clinical relevance of this approach. Cost and cold‑chain requirements, though, limit liposome use in the very regions that would benefit most from a simpler delivery method. Transdermal patches sidestep both the gastrointestinal tract and cold storage, providing a steady release that can span several days. The University of Texas polymer‑matrix patch achieved a 30 % increase in overall exposure, which could translate into fewer dosing events in mass‑drug campaigns. Skin irritation and the limited drug load per patch are practical concerns that formulation scientists must address through excipient optimization. Inhalable powders and nebulized solutions target respiratory infections directly, offering rapid onset and high local concentrations while keeping systemic exposure modest. Pre‑clinical ferret data revealed lung tissue levels four times higher than oral dosing, an encouraging sign for antiviral applications. Nevertheless, the need for proper inhalation devices and patient training may pose logistical hurdles in low‑resource settings. Implantable depot systems, borrowing concepts from veterinary medicine, could provide months‑long protection with a single insertion, ideal for mass prophylaxis. Ultimately, the best strategy may involve a hybrid approach, selecting the delivery platform that aligns with the specific disease, patient population, and infrastructure available.