Switching from a generic medication back to the brand-name version isn’t as simple as asking your pharmacist for the original pill. It’s a medical decision that needs careful planning, clear documentation, and often, a battle with insurance. Many people assume generics and brand drugs are identical-because they’re supposed to be. But for some, the difference isn’t just in price. It’s in how they feel.
Why You Might Need to Switch Back
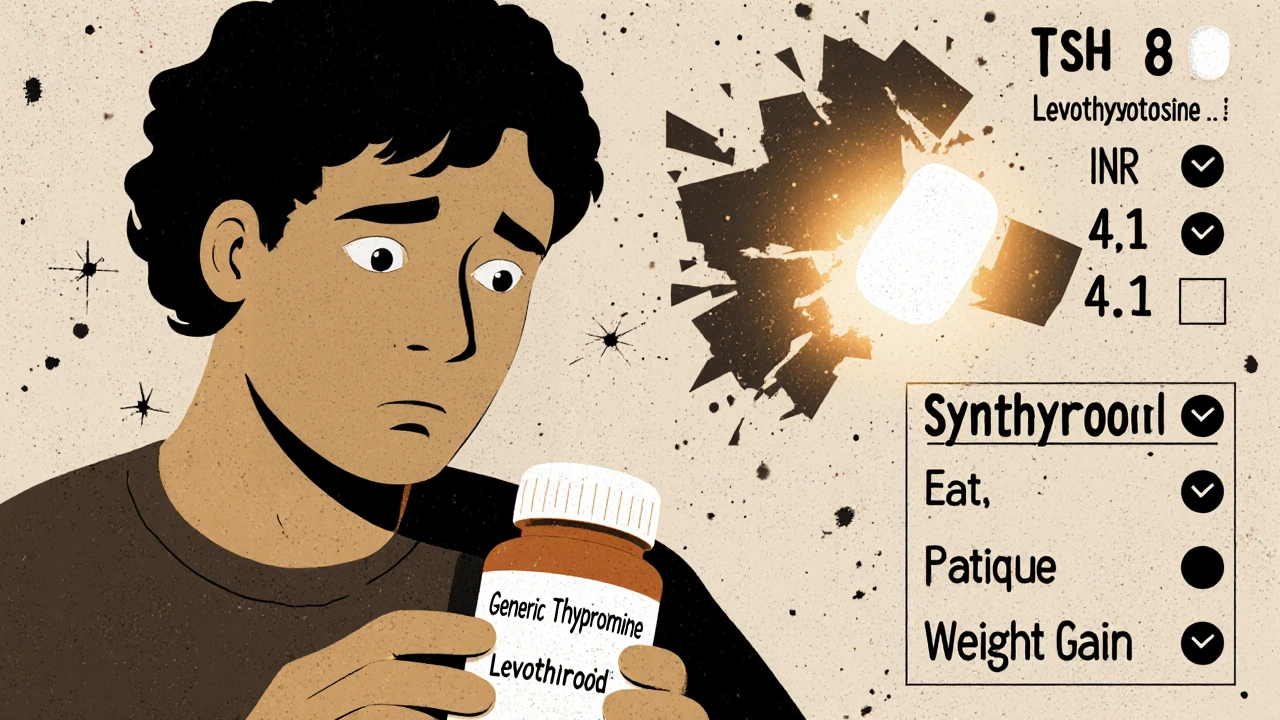
Generics are required by the FDA to have the same active ingredient, strength, and dosage as the brand-name drug. That’s the law. But what’s not required to be the same? The fillers, dyes, binders, and coatings-the inactive ingredients. These can trigger reactions in sensitive people. Real cases show up in clinics every week. A patient on generic levothyroxine starts feeling fatigued, gaining weight, or having heart palpitations-even though their dose hasn’t changed. A person on generic warfarin sees their INR levels swing wildly, putting them at risk for clots or bleeding. Someone with epilepsy has a breakthrough seizure after switching to a different generic version of lamotrigine. These aren’t rare. Studies show that for drugs with a narrow therapeutic index-where the difference between an effective dose and a toxic one is tiny-switching between different generic versions or back to brand can cause real problems. The FDA calls this out in its 2019 guidance. Drugs like warfarin, levothyroxine, phenytoin, cyclosporine, and lithium fall into this category. For these, even small changes in how the drug is absorbed can be dangerous.When Switching Back Is Medically Necessary
Not every complaint about a generic means you need the brand. But there are clear red flags:- You had stable control on the brand, then switched to a generic-and your condition worsened.
- You developed a new rash, swelling, or allergic reaction after switching to a generic.
- Your lab numbers (like INR, TSH, or drug levels) became unstable after the switch.
- You’re on a narrow therapeutic index drug and your doctor has seen similar cases before.
How to Get Your Doctor to Help
You can’t just walk into a pharmacy and ask for the brand. Pharmacists are legally allowed to substitute generics unless the prescriber says "Dispense as Written"-or DAW-1. Here’s what you need to do:- Track your symptoms. Write down exactly what changed: sleep, energy, mood, lab results, side effects. Date them. Bring this to your doctor.
- Ask for a formal switch request. Say: "I need to switch back to [Brand Name] because [generic] caused [specific issue]. Can you write a prescription with 'Brand Medically Necessary' on it?"
- Insist on the exact brand name. Don’t say "the original one." Say "Synthroid," not "levothyroxine." Say "Lipitor," not "atorvastatin." Generic manufacturers use different inactive ingredients-so even two different generics aren’t the same.
- Include lab results. If your INR jumped from 2.4 to 4.1 after switching generics, attach that report. If your TSH went from 2.1 to 8.7, include it. This isn’t optional-it’s what insurers require.

Insurance Will Fight You
This is where most people get stuck. Insurance companies don’t want to pay for brand-name drugs when generics exist. Medicare Part D denies 68% of brand requests unless there’s proof of medical necessity. Private insurers like Blue Cross Blue Shield deny even more-up to 82% in some cases. You need to be ready for a fight:- Ask your doctor to submit a prior authorization with your clinical data.
- If denied, appeal. Don’t stop there. The success rate for appeals with proper documentation is over 60%.
- Call your insurer. Ask: "What specific criteria do you need to approve this brand?" Write it down.
- Get help from a patient advocate. Many hospitals have them. Nonprofits like NeedyMeds or Patient Access Network Foundation can help with co-pay assistance.
What to Expect When You Get the Brand
Once you’re back on the brand, don’t assume everything’s fixed. Monitor yourself for the first week. Did your symptoms improve? Did your lab numbers stabilize? Did the rash go away? Keep taking your medication exactly as prescribed. Don’t switch again. Don’t try a different generic. If you had a reaction to one generic, you might react to another. Also, know this: brand manufacturers rarely change their inactive ingredients. Generics can-and do-switch suppliers, formulas, or dyes without telling you. One batch of generic levothyroxine might have a different filler than the next. The brand? It’s the same every time.What You Should Never Do
- Never switch yourself. Don’t ask your pharmacist to give you the brand without a doctor’s note. That’s not how it works.
- Never stop your meds. If you’re denied, don’t quit. Talk to your doctor about alternatives or temporary solutions.
- Never assume all generics are equal. A generic made by Teva isn’t the same as one made by Mylan-even if they’re both labeled "levothyroxine."
- Never ignore symptoms. If you feel off after a switch, speak up. Your body is telling you something.

When Switching Back Isn’t Recommended
For most people, generics work just fine. In fact, 92% of brand-to-generic switches are successful. The American Medical Association warns that many requests to switch back are based on perception, not science. If you’re stable, healthy, and your labs are good, there’s no reason to pay 3-5 times more. The American Academy of Neurology specifically advises against switching back and forth with anti-seizure drugs. One study found a 27% higher chance of breakthrough seizures when patients switched between different versions-even if one was the brand. And if you’re on a biologic-like Humira or Enbrel-the rules are even stricter. Biosimilars aren’t exact copies. Switching between them and the original brand can be risky and isn’t approved in many cases.What’s Changing in 2025
New rules are coming. Starting in 2024, Medicare Part D will have a new "Medically Necessary Brand Exception" pathway with a 72-hour approval guarantee for certain drugs. The FDA’s new GDUFA III rules require manufacturers to disclose formulation changes to prescribers. Pharmacies are also updating their systems. Most EHRs now have mandatory fields for "Brand Medically Necessary"-so if your doctor fills it out right, the system flags it automatically. But the biggest change? More patients are speaking up. And more doctors are listening.Final Thoughts
Switching back from a generic to a brand isn’t about being picky. It’s about safety. For some people, the difference between a generic and the brand isn’t just cost-it’s health. If you’ve had a bad reaction, your symptoms are real. Your doctor can help you get back on the right medication. But you have to be prepared to fight for it-with data, with documentation, and with persistence.The system isn’t perfect. But if you know your rights, your body, and your medical history-you can make it work.
Can I just ask my pharmacist for the brand name instead of the generic?
No. Pharmacists are legally allowed to substitute generics unless the prescription says "Dispense as Written" or "Brand Medically Necessary." If you ask for the brand without a doctor’s note, they’ll give you the generic. You need a written request from your prescriber to get the brand.
Will my insurance cover the brand if I switch back?
Maybe-but only if your doctor proves medical necessity. Most insurers require prior authorization with lab results, symptom logs, and a clear explanation of why the generic failed. Medicare and private plans deny up to 80% of initial requests. But if you appeal with solid documentation, approval rates jump to over 60%.
Are all generic drugs the same?
No. While generics must have the same active ingredient, their inactive ingredients-like dyes, fillers, and coatings-can vary by manufacturer. One generic version of levothyroxine might contain corn starch, while another uses lactose. These differences can affect absorption or trigger allergies. That’s why switching between generics-or back to brand-can cause problems, especially with narrow therapeutic index drugs.
Which drugs are most risky to switch between?
Drugs with a narrow therapeutic index are the most risky. These include warfarin (blood thinner), levothyroxine (thyroid), phenytoin and lamotrigine (anti-seizure), cyclosporine (transplant), and lithium (mood stabilizer). For these, even small changes in how the drug is absorbed can lead to serious side effects or loss of effectiveness.
What if my doctor won’t write the prescription for the brand?
Ask them why. If they say "it’s the same drug," ask them to show you clinical evidence that your reaction isn’t real. Bring your symptom log and lab results. If they still refuse, consider getting a second opinion from a specialist familiar with your condition. Some endocrinologists, neurologists, and cardiologists see these cases regularly and know how to advocate for you.
How long does it take to get approval for a brand-name drug?
It can take anywhere from 24 hours to two weeks. Medicare Part D claims average 14.3 days for prior authorization approval. But under the new 2024 rules, certain categories now have a 72-hour guarantee. If you’re running out of medication, tell your doctor-they may be able to give you a short-term supply while the approval is processed.
Can I switch back to the brand if I’m on Medicaid?
Yes, but the rules vary by state. Most Medicaid programs require prior authorization for brand-name drugs when generics are available. However, if you have documented therapeutic failure or an allergic reaction, your doctor can request an exception. Some states have specific policies for narrow therapeutic index drugs that make approval easier.
Are brand-name drugs more effective than generics?
For most people, no. Generics are required to be bioequivalent to the brand. But for a small group of patients-those with allergies to inactive ingredients, or those on narrow therapeutic index drugs-the brand may be more consistent and safer. Effectiveness isn’t about the active ingredient-it’s about how your body responds to the whole pill.
15 Comments
Michael SegbawuNovember 20, 2025 AT 01:44
Bro this is why america is falling apart nobody cares about real medicine anymore just cost cutting like we’re all robots or something
My cousin switched to generic levothyroxine and started having heart spasms like a damn cartoon character
Doctor laughed at her said it was all in her head
She almost died and now she’s on Synthroid again and fine
Insurance denied her 3 times
They need to burn the pharmacy boards
Aarti RayNovember 21, 2025 AT 08:29
in india we dont even have proper generics some times
my aunt took generic warfarin and her legs swelled like balloons
no one checks the fillers here
doctor just says same medicine same price
but body knows
we need more awareness
not just in usa
Alexander RolsenNovember 22, 2025 AT 18:45
This is exactly why I hate the FDA. They treat patients like lab rats. You have a documented reaction? Irrelevant. You have data? Doesn’t matter. The system is designed to ignore you until you’re in the ER. And then they’ll say, ‘We told you so.’Leah DoyleNovember 23, 2025 AT 02:32
This is so important and I’m so glad someone wrote this
I had the exact same thing with lamotrigine
Switched to generic and had a seizure in my kitchen
My mom called 911
They didn’t believe me when I said it was the pill
But when I showed them my old TSH and INR logs from before the switch…
They finally listened
Thank you for saying this out loud 💙
Alexis MendozaNovember 23, 2025 AT 22:36
It’s not about brand vs generic
It’s about consistency
Our bodies aren’t machines that can handle random changes in fillers
Think of it like eating the same bread every day
Then one day it’s made with a different flour
Maybe it’s gluten-free
Maybe it’s got a new preservative
You don’t know why you feel weird
But you feel weird
And that’s enough to matter
Michelle N AllenNovember 24, 2025 AT 16:27
I read this whole thing and honestly I’m tired
Why do we have to fight so hard for something that should be basic
Like if your car starts making a noise after you change the oil you don’t just accept it
You take it back
But with medicine you’re the bad guy for asking
And now I’m just gonna take my pills and shut up
Because I don’t have the energy
Madison MaloneNovember 25, 2025 AT 11:28
You’re not alone
I’ve been there
My doctor didn’t believe me either until I brought in my 6-month log of symptoms and lab results
It took 3 months but they approved Synthroid
And now I sleep again
And I’m not crying for no reason
It’s not weakness to need the brand
It’s science
You’re not crazy
You’re just not a number in their spreadsheet
Graham Moyer-StrattonNovember 26, 2025 AT 01:52
The system is broken. The FDA is a puppet. Generics are a corporate lie. Your body is the only truth.tom charltonNovember 27, 2025 AT 14:20
Thank you for this comprehensive and clinically grounded overview.
As a healthcare professional, I can confirm that the pharmacokinetic variability in certain generics-particularly for narrow therapeutic index medications-is well-documented in peer-reviewed literature.
Patients deserve individualized care, not cost-driven substitution.
Advocacy, documentation, and persistence are not luxuries-they are medical necessities.
And yes, the 72-hour Medicare exception pathway is a meaningful step forward.
Jacob Hepworth-wainNovember 29, 2025 AT 07:50
My dad had the same issue with cyclosporine after his transplant
Switched to generic and his levels dropped like a rock
They almost lost him
Now he’s on the brand and stable
Don’t let anyone tell you it’s all the same
Your body knows
And if it’s screaming
Listen
Craig HartelNovember 30, 2025 AT 12:50
Hey I just want to say this post gave me hope
I’ve been scared to speak up because I thought I was just being dramatic
But now I’m printing out my symptom log and taking it to my endo tomorrow
Thank you for making me feel like I’m not crazy
And if anyone needs help filling out forms I’ll help you
Just DM me
We got this 💪
Chris KahanicDecember 1, 2025 AT 14:37
Interesting data. The FDA’s 2019 guidance does acknowledge bioequivalence variability in certain drug classes.
However, the clinical significance remains debated in peer-reviewed journals.
Most meta-analyses show no statistically significant difference in outcomes for the general population.
That said, individual variation is real and should not be dismissed.
Context matters.
Geethu EDecember 1, 2025 AT 16:46
in my country we dont even have proper pharmacy records
one day you get generic from Cipla next day from Sun Pharma
no one tells you
my sister had seizures after switching
they blamed her for not taking it right
but the pill looked different
same name different color
same dose different soul
we need to fight for transparency
not just in usa but everywhere
anant ramDecember 3, 2025 AT 08:36
Thank you for sharing this detailed and much-needed guide!
As someone who has navigated insurance denials for brand-name medications, I can confirm: documentation is everything.
Always include lab results, symptom timelines, and physician notes.
Appeals are not just a formality-they are your lifeline.
And never, ever accept a pharmacist’s word over your doctor’s clinical judgment.
Knowledge is power-and you are not alone.
Michael SegbawuDecember 4, 2025 AT 21:13
Ugh I just saw this comment from some guy saying "meta-analyses show no difference"
Yeah sure buddy
My cousin’s heart stopped because your meta-analysis didn’t count her
Try telling that to her funeral
People aren’t data points
We’re people
And we’re tired of being ignored